Author Affiliations
Abstract
Introduction: Clinical auditing practices are recognized universally as a useful tool in evaluating and improving the quality of care provided by a health service.
Methodology: We assessed the quality of weekly handover practices of trauma patients in our orthopedic department, implemented changes, and re-assessed for improvement. We undertook a prospective study using the Royal College of Surgeons of England’s advice on safe handovers as minimal requirements, which include name, date of birth, patient location, responsible consultant, resuscitation plan, current diagnosis, operational issues like intensive care unit (ICU) beds availability, and results of pending investigations.
Results: A total of 20 admissions were investigated during the first week (May 01, 2021, to May 07, 2021). The standard in general of handover was very unsatisfactory, particularly, date of admission (42%), responsible consultant name (28%), condition of the patient at time of handover (47%), name of patient (66%), operational issues (61%), result of pending investigations (76%) were all under the expected standard (80%). After the Implementation of the electronic handover proforma, it was examined again for a one-week period (June 20, 2021, to June 26, 2021). This time, 25 patients were included in the process. There is only one criterion to fall under the standard 95% was the results of pending investigations (84%). The electronic proforma was used 100%.
Conclusion: The handover of trauma admissions was significantly enhanced and reduced the risk to patients. This tool has been shown to be a rapid, simple, accurate, and cost-effective method to improve communication in a complex, large trauma center.
Keywords
Handover, Trauma, Orthopedics, Royal College of Surgeons, Trauma care transition.
Introduction
Clinical auditing is widely acknowledged as a vital tool for assessing and enhancing healthcare quality globally.[1] A multidisciplinary Clinical Board plays a crucial role in developing and disseminating evidence-based clinical policies, while also monitoring their implementation to ensure optimal quality and safety outcomes.[2] The heterogeneous nature of patient presentations in emergency departments necessitates meticulous handovers to guarantee comprehensive continuity of care.[3] The transition of patient care to incoming teams constitutes a high-risk phase, wherein suboptimal communication can compromise patient safety.[4] Consequently, the delivery of effective handovers is an indispensable obligation for all healthcare providers.
Handovers between healthcare teams have been identified as a critical vulnerability in patient care pathways. In response, the Royal College of Surgeons (RCS) has developed and published evidence-based guidelines on optimal handover practices, providing a framework for standardized and effective communication.[5] Khyber Teaching Hospital, a premier university hospital and primary teaching affiliate of Khyber Medical College in Peshawar, Pakistan, serves as a major hub for trauma care. Despite being one of the largest hospitals in the country, the trauma unit is managed by only two trainee medical officers (TMOs), with on-call support from senior registrars and consultants.
This study aimed to evaluate the quality of weekly handover practices for trauma patients in our department, implement improvements, and reassess for enhanced patient safety and trainee education. By standardizing handovers, we sought to provide trainees with a structured template for capturing critical patient information, while also generating valuable data for future audits.
Background: As a tertiary healthcare facility, Khyber Teaching Hospital (KTH) serves as a major referral center for orthopedic trauma cases in the region. The trauma unit operates 24/7, with two TMOs responsible for managing a high volume of orthopedic emergencies, supported by on-call senior registrars and consultants. Two critical handover sessions occur daily: morning (8 am-8 pm) and night (8 pm-8 am) shifts. However, the junior TMO covering trauma often had limited experience, making it challenging to determine essential clinical information for efficient handovers.
The combination of variables led to inadequate handovers, informal, and patients were frequently not handed off at all. This posed a significant systemic risk to patients and junior staff. To address this issue, we aimed to standardize and improve the handover process by developing a specialized proforma tool.
Methodology
Improving trauma handovers: A quality improvement initiative. We identified some concerns regarding the standard of handovers and their possible effect on patient care as members of the Trauma team. To address this, we conducted a prospective study over a one-week period, using the Royal College of Surgeons of England guidance as the minimum criteria for safe handovers.
Initial findings and intervention: Our initial data revealed suboptimal handover practices. We presented our findings at the hospital’s Clinical Audit Committee and collaborated with stakeholders to develop a Trauma-specific written handover proforma. This proforma was introduced to ensure all admissions were officially recorded, and effective communication was facilitated between day and night teams.
Implementation and feedback: Trainees were educated on the proforma and expected handover standards through multimedia sessions. Initial feedback was positive, and our findings were presented in poster format at the hospital’s Patient Safety Conference. We reviewed our progress with the Clinical Audit Committee and decided to introduce an electronic version of the proforma, accessible from any hospital computer, in collaboration with the IT department.
Outcome and future directions: The electronic proforma was well-received by trainees, who reported improved continuity of care and handover processes. We assessed the quality of weekly handover practices, implemented changes, and re-assessed for improvement. Our initiative demonstrates the effectiveness of a structured handover proforma in enhancing patient care and highlights the importance of ongoing quality improvement in healthcare settings.
Results
First data: A total of 20 admissions were audited during the first week (May 01, 2021, to May 07, 2021), revealing a disappointing overall standard of handover. Specifically, key elements such as responsible consultant name (28%), date of admission (42%), patient condition at handover (47%), operational issues (61%), patient name (66%), and pending investigation results (76%) all fell short of the expected 80% compliance standard, highlighting significant room for improvement in the handover process.
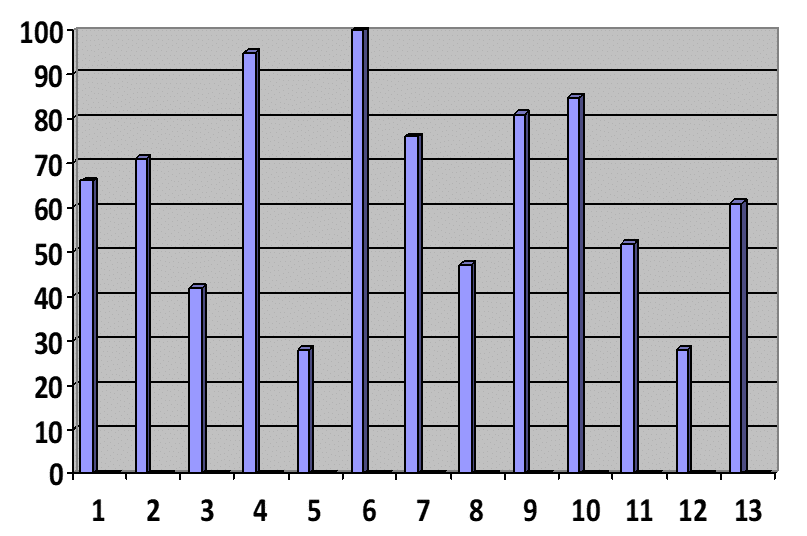
Figure 1: First data results: Name(1), age(2), date of admission(3), location(4), responsible consultant name(5), diagnosis(6), pending investigations(7), conditions of patient(8), urgency of care(9), management plan(10), resuscitation plan(11), consultant contact details(12), operational issues(13)
Second data: Following the introduction of the handover proforma, we conducted a re-evaluation of Trauma admissions over a one-week period (May 17, 2021, to May 23, 2021), encompassing 18 patients. The results showed a marked improvement in handover quality. Notably, two criteria fell short of the 80% standard: Management plan (70%) and Results of pending Investigations (45%). Encouragingly, adherence to the paper proforma was achieved at a rate of 100%.
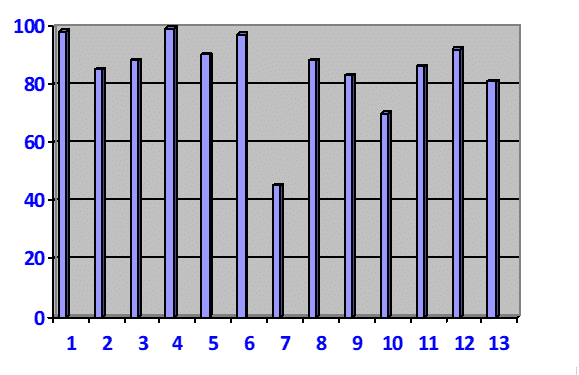
Figure 2: Second data results: Name(1), age(2), date of admission(3), location(4), responsible consultant name(5), diagnosis(6), pending investigations(7), conditions of patient(8), urgency of care(9), management plan(10), resuscitation plan(11), consultant contact details(12), operational issues(13)
Final data results: Following the implementation of the electronic handover proforma, a further evaluation was conducted over a one-week period (June 20, 2021, to June 26, 2021), incorporating 25 patients. The results demonstrated a sustained high standard of handovers, with only one criterion falling below the 95% target: results of pending investigations (84%). Notably, the uptake of the electronic proforma remained at 100%. The Trauma team provided positive feedback, praising the proforma for maintaining excellence in care and facilitating concise, clinically relevant handovers among cross-covering trainees.
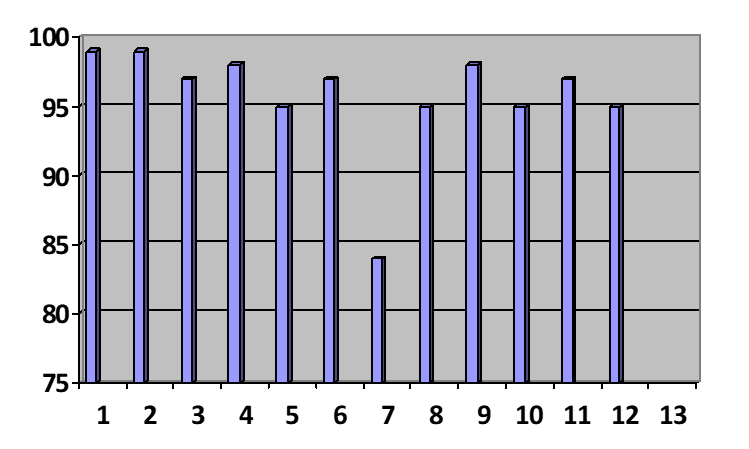
Figure 3: Final data: Name(1), age(2), date of admission(3), location(4), responsible consultant name(5), diagnosis(6), pending investigations(7), conditions of patient(8), urgency of care(9), management plan(10), resuscitation plan(11), consultant contact details(12), operational issues(13)
Discussion
The implementation of the electronic handover proforma has significantly enhanced the quality of trauma admission handovers in our unit, thereby reducing associated risks. This tool has proven to be a simple, accurate, and cost-effective method for improving communication in our tertiary care trauma center. Its reproducibility and versatility make it applicable to various specialties, and the findings of this study will inform future research and quality improvement initiatives.
This audit highlighted areas for improvement, which were subsequently addressed through targeted teaching sessions. The audit cycle has proven to be a valuable tool in monitoring, assessing, and enhancing clinical practice, ultimately ensuring the delivery of optimal patient care.[6] As demonstrated by this audit, implementing a standardized management protocol can effectively facilitate quality improvement and enhance patient management, particularly in high-pressure settings like the emergency department, where seamless handovers are crucial.[7]
This research makes a significant contribution by identifying and categorizing crucial factors within routine handover documentation that influence priority patient selection decisions.[8] Analysis revealed several factors significantly associated with patient outcomes.[9] Interestingly, this study also underscores the importance of audits as a tool for quality improvement, rather than merely a requirement for specialist training program entry, as previously suggested.[10]
To enhance the effectiveness of clinical audits, it is essential that auditors receive comprehensive training in clinical audit methodology and that audit departments provide ongoing support throughout the audit process.[2] Despite the widely acknowledged theoretical benefits of audits, a growing body of evidence suggests that their practical implementation often falls short of expectations.[11]
The implementation of the electronic handover tool at Khyber Teaching Hospital has yielded significant improvements in the handover of Trauma admissions, ultimately reducing patient risk. This innovative tool has proven to be a straightforward, efficient, cost-effective, and accurate means of enhancing communication within our complex trauma center. Notably, this attribute improvement effort is highly replicable and has wide significance across all the specialties and teams, with the results ready to guide future research endeavors.
Recommendations: Based on our study’s findings, we recommend the following:
- Adoption of standardized handover proformas: Healthcare institutions should consider implementing standardized handover proformas, tailored to their specific needs, to improve communication and reduce errors.
- Electronic implementation: Electronic proformas can enhance accessibility, usability, and consistency, and should be considered for widespread adoption.
- Training and education: Healthcare professionals should receive comprehensive training on the use of handover proformas to ensure effective implementation.
- Regular audits and feedback: Regular audits and feedback mechanisms should be established to monitor and improve handover practices.
Limitations: While our study demonstrates the effectiveness of a standardized handover proforma, several limitations should be acknowledged:
- Single-center study: Our study was conducted in a single tertiary care hospital, and the findings may not be generalizable to all healthcare settings.
- Limited sample size: Although our sample size was sufficient for the study’s objectives, larger studies may be needed to confirm the findings.
Study strengths: Despite these limitations, our study has several strengths:
- Prospective design: Our study’s prospective design allowed for a comprehensive evaluation of handover practices before and after the implementation of the proforma.
- Standardized intervention: The use of a standardized proforma ensured consistency in the intervention, enabling a fair evaluation of its effectiveness.
- Measurable outcomes: Our study’s outcomes were measurable, allowing for a quantitative assessment of the proforma’s impact on handover quality.
By addressing the limitations and building on the strengths, future studies can further refine the implementation of standardized handover proformas and explore their impact on patient outcomes.
Implications and boundary: While no online system or proforma may replace the effective communication between professionals, our study shows that well-designed adjuncts and simple ones may significantly increase the handover quality and eventually improve the patient care and reduce risk. The creation of our proforma provided valuable training opportunities for trainees, enabling them to identify key priorities for handover of acute trauma admissions quickly. Cross-covering trainees, in particular, reported feeling better prepared to present admissions.
Implementation challenges were primarily related to establishing a hospital-wide online proforma accessible on all computers. However, once overcome, our electronic tool proved extremely effective. Notably, proper training on its use was crucial, and collaboration with the IT department ensured a smooth resolution.
Conclusion
In conclusion, our study demonstrates that the implementation of a standardized electronic handover proforma significantly improves the quality of trauma admission handovers in our tertiary care hospital. The initial audit revealed suboptimal handover practices, which were substantially enhanced following the introduction of a paper-based proforma and further optimized with the electronic version. Our findings highlight the importance of structured communication tools in reducing patient risk and improving continuity of care. The electronic handover proforma has proven to be a simple, efficient, and cost-effective means of enhancing communication within our trauma center. Given its replicability and versatility, we recommend its adoption across various specialties and healthcare settings to standardize handover practices and improve patient safety.
References
- Berk M, Callaly T, Hyland M. The evolution of clinical audit as a tool for quality improvement. J Eval Clin Pract. 2003;9(2):251-257. doi:10.1046/j.1365-2753.2003.00389.x
PubMed | Crossref | Google Scholar - Glazebrook SG, Buchanan JG. Clinical governance and external audit. J Qual Clin Pract. 2001;21(1-2):30-33. doi:10.1046/j.1440-1762.2001.00390.x
PubMed | Crossref | Google Scholar - Wilson R. Improving clinical handover in emergency departments. Emerg Nurse. 2011;19(1):22-26. doi:10.7748/en2011.04.19.1.22.c8446
PubMed | Crossref | Google Scholar - Robertson A, Shrestha A. Achieving an effective handover is the duty of every doctor – is general surgical handover in a district general hospital compliant with the Royal College of Surgeons of England guidelines? Int J Surg. 2015;23(Suppl 1):S71. doi:10.1016/j.ijsu.2015.07.314
Crossref | Google Scholar - Lunt A, Yan S, Stones J. Improving weekend handover in trauma and orthopaedics: a four cycle audit. Int J Surg. 2015;23(Suppl 1):S86. doi:10.1016/j.ijsu.2015.07.389
Crossref | Google Scholar - Shah P, Badiani D, Davis D, Kalairajah Y. Improving the quality of orthopaedic elective and trauma operative notes: a completed audit loop study. Int J Surg Open. 2016;3:1-5. doi:10.1016/j.ijso.2016.04.005
Crossref | Google Scholar - Chan O. An audit on the management of patients with acute shoulder dislocation. Clin Audit. 2010;2:11-16. doi:10.2147/CA.S14229
Crossref | Google Scholar - Lim J, Churilov L, Smith P, Churilov I. Factors associated with patient selection for inpatient rehabilitation: an audit of decision-making in the rehabilitation assessment. Clin Audit. 2013;5:1-9. doi:10.2147/CA.S38904
Crossref | Google Scholar - Johnston E. Recycling the surgical audit. Clin Audit. 2010;2:89-92. doi:10.2147/CA.S12481
Crossref | Google Scholar - Kongnyuy E, Kabore A, Tebeu PM. Clinical audit to improve obstetric practice: what is the evidence? Clin Audit. 2009;1:1-9. doi:10.2147/CA.S6442
Crossref | Google Scholar - Scarparo S. Clinical audit, guidelines and standards: a productive relation for managing clinical practices. Financ Account Manag. 2011;27(1):83-101. doi:10.1111/j.1468-0408.2010.00517.x
Crossref | Google Scholar
Acknowledgments
We would like to thank Dr. Muhammad Imran Khan (Focal person for clinical audit, Department of Orthopedic Surgery) for his continuous support and expert input.
Funding
The authors received no financial support for the project, authorship, and/or publication of this article.
Author Information
Corresponding Author:
Sohail Rehman
Department of Orthopedic Surgery
Khyber Teaching Hospital Peshawar, Pakistan
Email: sann090909@gmail.com
Co-Authors:
Musawir Iqbal, Zia Ullah Jan, Asif Nawaz, Muhammad Imran Khan
Department of Orthopedic Surgery
Khyber Teaching Hospital Peshawar, Pakistan
Authors Contributions
Sohail Rehman contributed to the conceptualization, methodology, investigations, data curation, formal analysis, and drafting of the manuscript. He also led the research process, managed the project, presented it at the clinical audit meeting, and liaised with key stakeholders to implement the proposed changes. Musawer Iqbal contributed to the literature review and data collection. Zia Ullah Jan assisted with data collection and the refinement of the manuscript. Asif Nawaz provided support for the literature review and technical aspects of the study. Muhammad Imran Khan oversaw overall project monitoring, proposed recommendations to the hospital audit committee, and assisted in implementing the changes.
Ethical Approval
Ethical approval was not required for this study as it did not involve human or animal subjects.
Conflict of Interest Statement
The authors declare no conflicts of interest related to this work.
Guarantor
None
DOI
Cite this Article
Rehman S, Iqbal M, Jan ZU, Nawaz A, Khan MI. Trauma Care Transitions: A Clinical Audit in a Pakistani Tertiary Care Teaching Hospital. medtigo J Emerg Med. 2025;2(4):e3092241. doi:10.63096/medtigo3092241 Crossref









