Author Affiliations
Abstract
Background: Hypertension (HTN), the “silent killer,” is an ever-increasing global health concern, affecting a massive 1.28 billion adults worldwide. Alarmingly, over 50% of the hypertensives across the globe are unaware of their elevated blood pressure (BP). This undiagnosed HTN is a cause for concern, especially in developing countries like Pakistan that face constrained health resources. Our study aims to shed light on the prevalence of undiagnosed HTN among patients presenting to the outpatient departments (OPDs) of public tertiary hospitals in Rawalpindi, Pakistan. According to our knowledge, no similar hospital-based study has been conducted in Pakistan before.
Methodology: A descriptive, cross-sectional study was conducted in May 2024 on 148 OPD patients of three tertiary hospitals in Rawalpindi, Pakistan. Prevalence of HTN was measured, and its association with different demographic variables of the population was analyzed.
Results: Out of the 148 participants of the study, around 30% were diabetic, and 13% were smokers. Undiagnosed HTN and prehypertension (PHTN) were present in 22% and 40% of the patients, respectively. Gender and diabetes status were significantly associated with HTN; females and diabetics had a higher mean blood pressure (MBP). Females had 2.8 times higher chances of having undiagnosed HTN than males. A p-value of <0.05 and a 95% confidence interval (CI) were adopted for all analyses.
Conclusion: This study concluded that the 22% prevalence of undiagnosed HTN is alarming, and it should serve as a catalyst for the institution of an adequate BP monitoring set-up in the OPDs of public tertiary hospitals in Rawalpindi, Pakistan.
Keywords
Prevalence, Hypertension, Prehypertension, Blood pressure, Tertiary hospital, Non-communicable diseases.
Introduction
HTN, also known as the “silent killer,” has long been a global health problem, causing human suffering as well as a financial burden on the economies of various countries. It stands as a leading culprit in premature mortality worldwide, affecting a massive 1.28 billion adults, with its consequences worsening dramatically.[1] A comprehensive meta-analysis by the non-communicable diseases (NCDs) Risk Factor Collaboration reveals a twofold increase in the global prevalence of HTN between 1990 and 2019.[2]
Low- and middle-income countries bear the brunt of HTN, with two-thirds of all cases occurring in these regions, posing significant challenges for healthcare systems and patients alike.[3] Meanwhile, more than 50% of the Southeast Asian hypertensives are undiagnosed, emphasizing the need for increased awareness.[4] In Pakistan, the situation is equally concerning, with a significant proportion of adults remaining undiagnosed and untreated for HTN. A study from the second national diabetes survey of Pakistan (NDSP) revealed that 21.3% of the participants received a new diagnosis of HTN.[5]
HTN is an iceberg disease, with many cases hidden from view. People with undiagnosed HTN make up the unseen part of the iceberg.[6] In its early stages, HTN is often a silent condition, with symptoms going unnoticed.[7] This emphasizes the importance of screening efforts to ensure prompt diagnosis. However, many public tertiary hospitals in Pakistan largely neglect BP monitoring, despite the ease of doing so in a clinical setting. This study aims to determine the prevalence of undiagnosed HTN among patients visiting the OPDs of three public tertiary hospitals in Rawalpindi, Pakistan. We are aware of no similar hospital-based study conducted previously in Pakistan. Consequently, this study aims to underscore the importance of BP checks for patients presenting to the OPDs of such hospitals.
Methodology
Study design and settings: This descriptive cross-sectional study is based in the OPD setting of three public tertiary hospitals in Rawalpindi, Pakistan.
Target population: The study included patients over 18 years of age who presented to the OPD of public tertiary hospitals in Rawalpindi for various ailments. Patients who were already diagnosed with HTN, patients who were taking any anti-hypertensive medication, patients who were pregnant, and patients who were not in a physical or mental condition to have their BP monitored were excluded from the study.
Sample size and sampling: Based on the assumption of a 10.1% (p) prevalence of undiagnosed HTN in a previously conducted screening program, the Cochran formula was used to calculate the sample size (with a 95% CI and a 5% margin of error).[6] The sample size was calculated to be 139. The study employed simple random sampling techniques. In May 2024, we monitored the BP of a total of 148 patients.
Data collection: We used a previously validated questionnaire to collect data on the participants’ age, gender, history of diabetes, HTN, and smoking history. A standard OMRON digital BP monitor was used to minimize variations among different individuals. The patients were seated comfortably with their arms at the level of their chests. We took two BP readings on the same arm, documented the meaning of the two readings, and used them for analysis. A reasonable time gap between the two readings was ensured. We trained the health care personnel adequately, recording the BP of patients beforehand to ensure consistency in the results. Patients with elevated BP were advised to consult a relevant healthcare professional at the hospital for a thorough evaluation.
Statistical analysis: We used the Statistical Package for the Social Sciences (SPSS) version 27 for data entry, coding, and analysis. Descriptive statistics were used to analyze the sample characteristics, and categorical variables are represented as frequencies (percentages). We applied Pearson’s chi-squared test to examine the association between the previously defined BP categories and the participants’ gender, diabetes, and smoking status. For significant variables, we performed binary logistic regression analysis using no HTN and undiagnosed HTN as outcome variables. For this test, normal BP and PHTN were recorded into the single category of no HTN. We also conducted an independent sample t-test to compare the average of the MBP of males and females, diabetics and non-diabetics, and smokers and non-smokers. We calculated each participant’s MBP using the following formula: MBP = Diastolic Blood Pressure (DBP) + 1/3 (systolic blood pressure (SBP) minus DBP), where SBP represents systolic blood pressure and DBP represents diastolic blood pressure. A value of p < 0.05 and a 95% confidence interval were adopted for all analyses. There were no missing values.
Results
The study involved a total of 148 patients, 48% (n = 72) males and 51% (n = 76) females (Table 1). The majority of the patients were in the age group 50–59 (23%), while the mean age group of the participants was 40–49 (17%). Approximately 30% of participants were diabetic, and 13% were smokers. Table 2 represents the distribution of participants based on their socio-demographic characteristics into the three categories of BP: normal BP, PHTN, and HTN.
In our study, the prevalence of undiagnosed HTN was 22%, while around 40% of the participants had PHTN (Figure 1). Out of the 33 hypertensive patients, there were 10 male and 23 female hypertensive patients. Most of the hypertensive patients (30%) belonged to the age group 50–59. Pearson’s chi-square test showed that BP was significantly associated with the participants’ gender (p = 0.017) and the diabetes status of the participants (p = 0.012). But the association between BP and age (p = 0.130) and smoking status (p = 0.451) was significant.
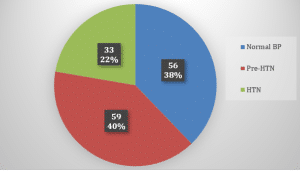
Figure 1: Prevalence of undiagnosed HTN among the patients presenting to the OPD of tertiary care hospitals in Rawalpindi, Pakistan
| Age category in years | Gender | Total | |
| Male (%) | Female (%) | ||
| 20-29 | 14 (19.4) | 19 (25.0) | 33 |
| 30-39 | 12 (16.7) | 21 (27.6) | 33 |
| 40-49 | 15 (20.8) | 11 (14.5) | 26 |
| 50-59 | 18 (25.0) | 17 (22.4) | 35 |
| >60 | 13 (18.1) | 8 (10.5) | 21 |
| Total | 72 (100) | 76 (100) | 148 |
Table 1: Age and gender distribution of study participants
| Variables | Number of participants with normal BP (%) | Number of participants with pre-HTN (%) | Number of participants with HTN (%) | Total (n=148) |
| Age | ||||
| 20-29 | 19 (33.9) | 10 (16.9) | 4 (12.1) | 33 |
| 30-39 | 14 (25.0) | 12 (20.3) | 7 (21.2) | 33 |
| 40-49 | 10 (17.9) | 11 (18.7) | 5 (15.) | 26 |
| 50-59 | 7 (12.5) | 18 (30.5) | 10 (30.3) | 35 |
| >60 | 6 (10.7) | 8 (13.6) | 7 (21.2) | 21 |
| Gender | ||||
| Male | 26 (46.4) | 36 (61.0) | 10 (30.3) | 72 |
| Female | 30 (53.6) | 23 (39.0) | 23 (69.7) | 76 |
| Current tobacco use | ||||
| Yes | 10 (17.9) | 7 (11.9) | 3 (9.1) | 20 |
| No | 46 (82.1) | 52 (88.1) | 30 (90.9) | 128 |
| Diabetes status | ||||
| Yes | 10 (17.9) | 25 (42.4) | 8 (24.2) | 43 |
| No | 46 (82.1) | 34 (57.6) | 25 (75.8) | 105 |
Table 2: Socio-demographic variables of the study population (Data presented as n (%))
We conducted an independent sample T test to compare the means of the MBP for males and females. There was a significant difference (t(df) = 146, p<0.05) in the means. Females had a higher MBP (M = 96.8 mm of Hg, SD = 13.3 mm of Hg) than males (M = 92.8 mm of Hg, SD = 12.2 mm of Hg). The alternate hypothesis was accepted due to the significant magnitude of the mean difference. We also conducted an independent sample T test to compare the means of the MBP in diabetics and non-diabetics. The means showed a significant difference (t(df) = 146, p<0.05). The MBP for diabetics (M = 98.0 mm of Hg, SD = 11.3 mm of Hg) was higher than that for non-diabetics (M = 93.6 mm of Hg, SD = 13.3 mm of Hg). The alternate hypothesis was supported due to the significant magnitude of the mean difference. However, the mean difference in the MBP was not significant between smokers and non-smokers.
| Variable | Category | Undiagnosed HTN (%) | No HTN/ Normal BP (%) | Total (%) | OR | p-value | 95% CI | |
| LL | UL | |||||||
| Gender | Male | 10 (13.9) | 62 (86.1) | 72 (48.6) | 2.831 | 0.030 | 1.109 | 7.231 |
| Female | 23 (30.3) | 53 (69.7) | 76 (51.4) | |||||
| Current tobacco use | Yes | 3 (15.0) | 17 (85.0) | 20 (13.5) | 0.909 | 0.899 | 0.210 | 3.948 |
| No | 30 (23.4) | 98 (76.6) | 128 (86.5) | |||||
| Diabetes status | Yes | 8 (18.6) | 35 (81.4) | 43 (29.1) | 1.470 | 0.407 | 0.592 | 3.650 |
| No | 25 (23.8)) | 80 (76.2) | 105 (70.9) | |||||
Table 3: Binary logistic regression analysis showing the odds ratio of association of gender with HTN (other variables are statistically insignificant), statistically significant at p<0.05
Lastly, we applied binary logistic regression analysis to all the variables associated with the outcome categories of no HTN and undiagnosed HTN (Table 3). The study found an independent relationship between gender and hypertension (OR = 2.831, p = 0.030), indicating a higher risk of undiagnosed HTN in females compared to males.
Discussion
The findings of this study revealed a 22% prevalence of undiagnosed HTN among the patients visiting the OPD of three tertiary hospitals in Rawalpindi. Our results are consistent with a previous large-scale survey on the prevalence of HTN in Pakistan, which reported a 21.3% prevalence of undiagnosed HTN.[8,9] It also shares similar results with Majumdar A et al.’s screening study at a primary health facility in India, where the prevalence of newly diagnosed HTN was 18%.[10] Sociodemographic, cultural, and dietary differences between the two regions account for the slight increase in the prevalence of HTN in our study as compared to the latter study. We determined that 40% of patients in our study are prehypertensive. This result aligns with the 37.7% regional prevalence of PHTN in India.[10] Once again, the differences in sampling methodology and geographical factors might have contributed to the minor differences observed between the two studies.
The high prevalence of PHTN and HTN in our society is probably due to a lack of awareness about the risk factors and prevention strategies for HTN. A range of risk factors, both modifiable and non-modifiable, influence the multifaceted condition of HTN. Non-modifiable risk factors include advancing age, family history, and low socioeconomic status. Conversely, we can modify behavioral risk factors such as smoking, excessive alcohol consumption, poor diet, high body mass index (BMI), excessive salt intake, physical inactivity, and stress to lower the risk of HTN.[11] Indifference towards avoiding these factors accounts for the alarming results of this study and of the other HTN screening programs conducted in our society.
As per our knowledge, various screening programs have previously surveyed the prevalence of diagnosed and undiagnosed HTN in the urban and rural areas of Pakistan. However, this study is unique because it is a hospital-based study as opposed to a community-based survey. Furthermore, our study has only accounted for the prevalence of undiagnosed HTN, excluding those with a prior diagnosis of HTN.
Our study also found that gender was significantly associated with BP, and females were more likely to be hypertensives than males. This was in conformity with the findings of the Shafi S et al. survey of HTN in Punjab, in which they found that women, as compared to men, were more hypertensive.[12] A possible interpretation for this observation is that women in our societal set-up lead a comparatively sedentary lifestyle as compared to men, and they also have a relatively higher prevalence of modifiable risk factors for HTN, such as stress and obesity, as compared to men. They are also more ignorant of their health, and dietary and lifestyle modifications for prevention of various NCDs, as compared to their male counterparts.
The results of our study showed that the prevalence of HTN was highest in the age group of 50–59 years. This result is also coherent with some previous studies, although Bansal S et al. reported that the most prevalent age group for HTN was 65–75 years.[13] The latter study was community-based, whereas this study is hospital-based, which might explain the difference.
Our study revealed that 18% of diabetic patients had undiagnosed HTN. This was a little higher than the Majumdar A et al. finding, which showed that 12% of diabetic patients were hypertensive.[10] However, Undavalli V et al. reported a closer result: 15%. Nevertheless, our study did not identify a relationship between smoking and HTN in an individual, like the findings of the Shafi et al. survey of HTN in Punjab. However, a similar study in India found a positive association between HTN and smoking.[7] The explanation for this difference is not clear.
To the best of our knowledge, this study is the pioneer of its type in the region. To date, an HTN screening study has not been conducted in any public tertiary hospital in Pakistan. Furthermore, our study highlights not only the prevalence of undiagnosed HTN but also the prevalence of PHTN among patients.
Limitations: We must acknowledge some limitations in this study. Firstly, the sample size was relatively small. Secondly, our study focused on patients visiting tertiary care hospitals in Rawalpindi, thereby limiting its generalizability to the entire Pakistani population despite the use of simple random sampling for data collection to reduce sampling bias. Moreover, our study conducted BP monitoring in a hospital setting, and we did not eliminate the possibility of ‘white-coat HTN in a patient with elevated BP. This could have led to an overestimation of the prevalence of HTN. Furthermore, the question of diabetes and smoking status relied on self-reporting by the participant, which could have led to bias. Finally, this study only screened out HTN; it did not confirm the diagnosis in an individual.
Recommendations: Future studies should focus on a comprehensive study on this topic in a similar hospital setting with a larger sample size. To minimize the possibility of ‘white coat HTN’ and diagnose HTN in an individual, BP should be measured at different times of the day, including once outside the hospital environment. Given the 22% prevalence of undiagnosed HTN in this study, efforts to raise public awareness about HTN are required; people should understand the importance of managing the modifiable risk factors for HTN. We should also devise strategies for early detection of HTN, with a primary focus on monitoring the BP of patients presenting to the OPDs of all government hospitals.
Conclusion
In conclusion, this study shows that the prevalence of undiagnosed HTN is 22% and the prevalence of PHTN is 40% among patients coming to the outpatient department of tertiary hospitals in Rawalpindi for various ailments. These alarming results highlight that there is a dire need for interventions to screen, control, and possibly reduce the burden of this disease. One of the most important interventions is to monitor the BP of every patient who presents to any public tertiary hospital’s OPD as a baseline test. For patients with high BP, follow-up, adequate diagnostic tests, dietary modification counseling, and, if necessary, medication should be ensured.
References
- World Health Organization. Hypertension. 2023. Hypertension
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 2021;398(10304):957–980. doi:10.1016/S0140-6736(21)01330-1 PubMed | Crossref | Google Scholar
- World Health Organization. Tonga Hypertension Fact Sheet. 2020. Tonga Hypertension Fact Sheet
- Hasan M, Tasnim F, Tariqujjaman M, et al. Examining the prevalence, correlates and inequalities of undiagnosed hypertension in Nepal: a population-based cross-sectional study. BMJ Open. 2020;10:e037592. doi:10.1136/bmjopen-2020-037592 PubMed | Crossref | Google Scholar
- Basit A, Tanveer S, Fawwad A, Naeem N, NDSP Members. Prevalence and contributing risk factors for hypertension in urban and rural areas of Pakistan: a study from the second National Diabetes Survey of Pakistan (NDSP) 2016–2017. Clin Exp Hypertens. 2019;41(7):597–604. doi:10.1080/10641963.2019.1619753 PubMed | Crossref | Google Scholar
- Undavalli VK, Mp H. Prevalence of undiagnosed hypertension: a public health challenge. Int J Community Med Public Health. 2018;5(4):1494–1498. doi:10.18203/2394-6040.ijcmph20180974 Crossref | Google Scholar
- Feng XL, Pang M, Beard J. Health system strengthening and hypertension awareness, treatment and control: data from the China Health and Retirement Longitudinal Study. Bull World Health Organ. 2013;92:29–41. doi:10.2471/BLT.13.124495 PubMed | Crossref | Google Scholar
- McElfish PA, Scott AJ, Chatrathi HE, et al. Undiagnosed hypertension and undiagnosed type 2 diabetes among overweight and obese Marshallese participants in a diabetes prevention program. Yale J Biol Med. 2021;94(1):5–12. Undiagnosed hypertension and undiagnosed type 2 diabetes among overweight and obese Marshallese participants in a diabetes prevention program
- U.S. Department of Health and Human Services. The Seventh Report of the Joint National Committee on High Blood Pressure Prevention, Detection, Evaluation, and Treatment. 2004. The Seventh Report of the Joint National Committee on High Blood Pressure Prevention, Detection, Evaluation, and Treatment
- Majumdar A, Chinnakali P, Daya PA, Shidam UG, Roy G. Opportunistic screening for hypertension and selected cardiovascular risk factors among adults attending a primary health center in Puducherry, India. Int J Prev Med. 2014;5(5):611–617. Opportunistic screening for hypertension and selected cardiovascular risk factors among adults attending a primary health center in Puducherry, India
- Ivičević Uhernik A, Kralj V, Čukelj P, et al. Undiagnosed hypertension exists in Croatia. Croat Med J. 2023;64(1):4–12. doi:10.3325/cmj.2023.64.4 PubMed | Crossref | Google Scholar
- Shafi ST, Shafi T. A survey of hypertension prevalence, awareness, treatment, and control in health screening camps in rural central Punjab, Pakistan. J Epidemiol Glob Health. 2017;7(2):135–140. doi:10.1016/j.jegh.2017.01.001 PubMed | Crossref | Google Scholar
- Bansal SK, Saxena V, Kandpal SD, et al. The prevalence of hypertension and hypertension risk factors in a rural Indian community: A prospective door-to-door study. J Cardiovasc Dis Res. 2012;3(2):117–123. doi:10.4103/0975-3583.95365 PubMed | Crossref | Google Scholar
Acknowledgments
The authors affirm that there is no external funding involved in this research project. Also, all the data used to generate the results is available in a Google form and can be provided on request.
Funding
There was no external funding for the research project.
Author Information
Corresponding Author:
Muhammad Majid Shafi
Department of Medicine
Rawalpindi Medical University, Rawalpindi, Pakistan
Email: majidshafi2001@gmail.com
Co-Authors:
Muhammad Umair, Muhammad Hammad Noor, Muhammad Ibrahim Shahzad
Department of Medicine
Rawalpindi Medical University, Rawalpindi, Pakistan
Aiman Latif Qureshi, Maryam Sial
Department of Medicine
Sheikh Zayed Medical College, Rahim Yar Khan, Pakistan
Sidra Hamid
Department of Physiology
Rawalpindi Medical University, Rawalpindi, Pakistan
Authors Contributions
All authors contributed to the conceptualization, investigation, and data curation by acquiring and critically reviewing the selected articles. They were collectively involved in the writing – original draft preparation and writing – review & editing to refine the manuscript. Additionally, all authors participated in the supervision of the work, ensuring accuracy and completeness. The final manuscript was approved by all named authors for submission to the journal.
Ethical Approval
The institutional review board (IRB) of Rawalpindi Medical University reviewed and approved the study (Ref No. 906/IREF/RMU/2024). We obtained informed consent from all participants and maintained complete confidentiality. Moreover, no misleading information is given. We avoided using deceptive methods and granted all participants the right to opt out of the study if they so desired. We accepted the request of some patients who simply had their blood pressure monitored but refused to include their data in the study.
Conflict of Interest Statement
The authors declare no conflict of interest.
Guarantor
None









