Author Affiliations
Abstract
Antiphospholipid syndrome (APS) is an autoimmune disorder characterized by recurrent thrombosis and/or pregnancy morbidity in the presence of specific antiphospholipid antibodies. This case report highlights the increasing prevalence of ischemic stroke in young adults and the diagnostic challenge it poses. We present the case of a 26-year-old male who suffered an acute ischemic stroke and was subsequently diagnosed with primary APS. His presentation included sudden right arm weakness, initially improving with antiplatelet therapy. However, persistent neurological findings, including hyperreflexia and bilateral dysmetria, prompted further investigation. Brain MRI revealed acute infarctions in both cerebellar and cerebral hemispheres, specifically bilateral periventricular and deep white matter infarcts consistent with watershed/border-zone involvement, and moderate small-vessel disease. Essentially, laboratory tests showed significantly elevated lupus anticoagulant (LA1 and LA2) levels, despite negative anticardiolipin and anti-β2 glycoprotein I antibodies, and the absence of other autoimmune disease markers. This led to a diagnosis of primary APS. Following an instantaneous diagnosis, the patient received long-term oral anticoagulation with warfarin, antiplatelet medication, and statins, resulting in significant neurological recovery. This case underscores the vital importance of evaluating for APS in young stroke patients without a history of other autoimmune diseases. Comprehensive laboratory assessment, including antiphospholipid antibody screening, is essential for accurate diagnosis and guiding appropriate, timely management to mitigate the risk of recurrent thrombotic events.
Keywords
Antiphospholipid Syndrome, Anti-cardiolipin antibodies, Ischemic Stroke, Thromboembolism, Antiphospholipid antibodies.
Introduction
Epidemiological evidence suggests that the prevalence of ischemic stroke in young individuals (18-50 years) has increased dramatically. These individuals have a long life expectancy following a stroke, which poses significant challenges to healthcare systems due to the high cost of long-term care.[1] The most prevalent brain disorder induced by APS is an ischemic stroke. Identifying patients with APS who are at high risk of suffering any thrombotic event continues to be a severe difficulty.[2] APS can be either primary or secondary, arising from another condition. Around 53% of cases are primary, with 36% after systemic lupus erythematosus. Other causes of APS include Sjogren’s syndrome, rheumatoid arthritis, systemic sclerosis, systemic vasculitis, and dermatomyositis. Primary and secondary APS have similar risks of pregnancy loss and arterial and venous thrombosis.[3,4]
APS can exhibit a wide range of clinical features. Deep vein thrombosis is the most common clinical feature (38.9%). Common symptoms include pulmonary embolism (14.1%), migraine (20.2%), livedo reticularis (24.1%), stroke (19.8%), arthralgia (38.7%), and valve malfunction (11.6%). Furthermore, around 35.4% of patients experience early fetal loss (<10 weeks).[1,5] APS is an autoimmune disease that causes vascular thrombosis and pregnancy complications. Specific antibodies, including anti-cardiolipin antibodies (aCL), anti-β2 glycoprotein I antibodies (anti-β2GPI), and lupus anticoagulant (LA), are detected in the blood. APS can occur in solitary (primary APS) or with other autoimmune diseases, including lupus (SLE).[4] Multiple organs can fail quickly due to tiny blood clots, which can be fatal in a severe type of APS known as catastrophic APS (CAPS).[3] APS has a powerful impact on cerebral circulation, and cerebrovascular condition is associated with significant mortality and morbidity, as well as critical and frequently severe consequences. Thus, one of APS’s primary therapeutic goals is to prevent recurrent thrombotic stroke.[4] Previous research has found a stronger association between antiphospholipid antibodies (APLA) and stroke in young people.[5,6] In this case report, we describe a 26-year-old male with primary APS who presented with an acute ischemic stroke. This highlights the necessity of addressing this condition in the differential diagnosis of young stroke patients.
Case Presentation
A 26-year-old man came in with a 20-day history of sudden weakness in his right arm, particularly noticeable in his right index finger. He had experienced heat stroke before these symptoms began, which were initially thought to be a complication of that incident. His condition improved significantly with antiplatelet therapy and physiotherapy. His cranial nerves and fundoscopy appeared normal on the examination, but he exhibited generalized hyperreflexia, bilateral dysmetria, prolonged clonus, and a positive right arm drift. The sensations were intact. Laboratory investigations revealed leukocytosis with neutrophilia, decreased HDL levels, elevated C-reactive protein (CRP), and increased erythrocyte sedimentation rate (ESR). The levels of LA1 and LA2 were elevated, with an increased ratio. Serum electrolytes, liver and renal function tests, and magnesium levels were normal. Antiphospholipid antibodies (anticardiolipin IgM/IgG, anti-β2 glycoprotein IgG/IgM) and other autoimmune markers such as extractable nuclear antigen (ENA), anti–cyclic citrullinated peptide (anti-CCP), cytoplasmic antineutrophil cytoplasmic antibody (cANCA), perinuclear antineutrophil cytoplasmic antibody (pANCA), and antinuclear antibody (ANA) were all negative. Protein C and protein S concentrations were normal. The MRI brain showed acute infarctions in both cerebellar hemispheres, as well as bilateral periventricular and deep white matter infarctions involving the frontal and parietal lobes, with restricted diffusion concerning for watershed infarct/border zone infarcts. Periventricular hyperintensities are likely suggestive of Fazekas Il change (Figure 1).
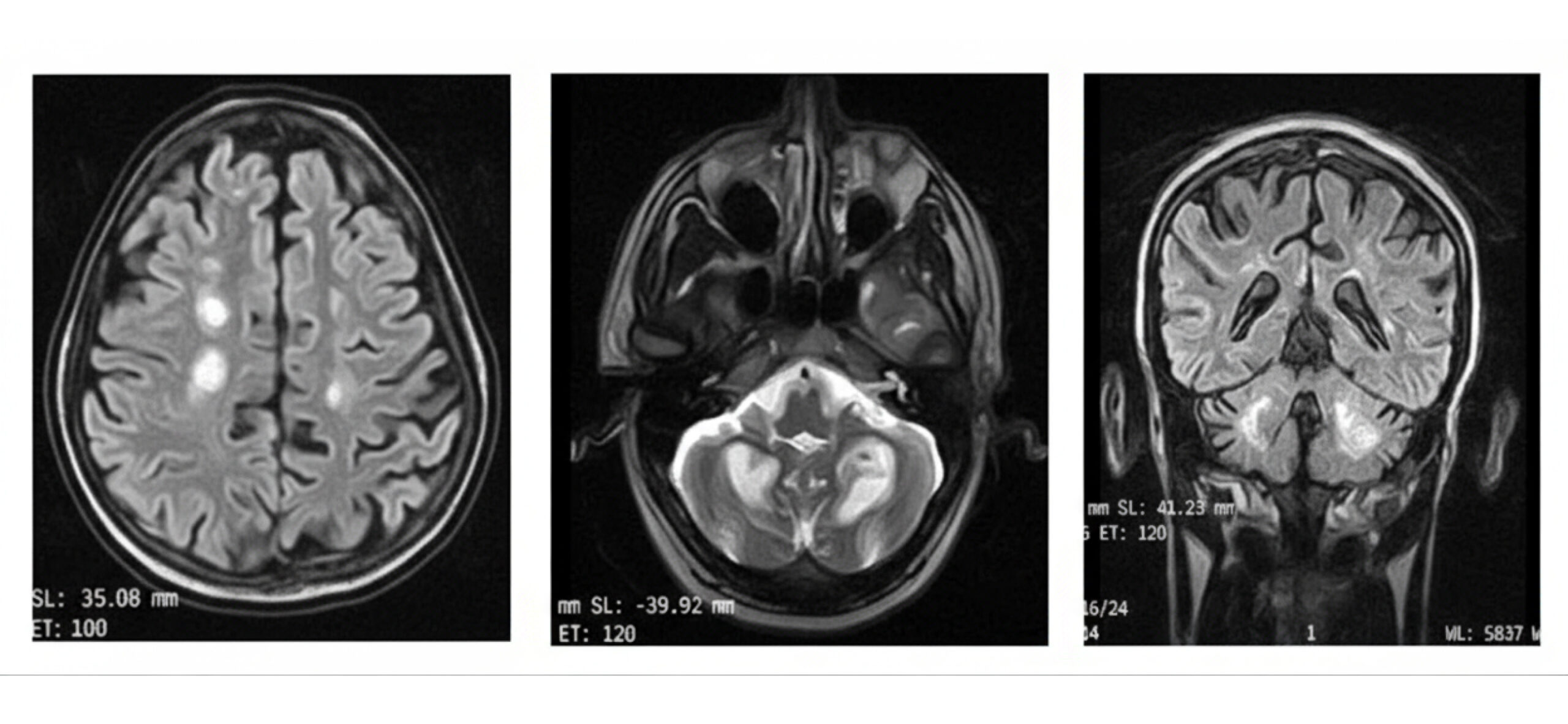
Figure 1: a) Acute cerebellar infarcts, left greater than right; b) Bilateral periventricular and deep white matter infarcts; c)Moderate small vessel disease (Fazekas grade II)
Based on their clinical presentation and laboratory results, the patient was diagnosed with APLA.
Case Management
The Rheumatology and Neurology teams were involved and recommended indefinite anticoagulation therapy with a Vitamin K antagonist (VKA), warfarin 5 mg per day, and targeting an International normalized ratio (INR) of 2.0–3.0. Prompt treatment with antiplatelet agents and statins led to significant neurological recovery.
Discussion
Antiphospholipid antibody syndrome is an autoimmune disorder identified by the presence of venous thromboembolism, arterial thrombotic complications, and pregnancy morbidities with the persistent presence of APLA, such as lupus anticoagulant, anti-β2-glycoprotein-I antibodies, and anticardiolipin.[1,4,7] These are autoantibodies that target phospholipid-binding proteins and fall into three types. Despite vivo extension, these antibodies cause in-vivo thrombosis in several organ systems.[6] Venous and arterial thrombosis are most prevalent in the lower limbs and cerebral artery circulation, respectively. However, thrombosis can develop in any organ. Catastrophic antiphospholipid syndrome is a serious condition with a high fatality rate. Treatment varies based on clinical presentation and antibody positivity.[8] After antiphospholipid antibodies are produced, cells like platelets, monocytes, neutrophils, and endothelial cells become active. These cells help form blood clots, and the most common problem caused by APS is transient or acute ischemic stroke.[9]
The abnormally functioning endothelium and the activation of some proteins by APL are major contributors to the creation of APS. The case report that follows, which concerns the patient below, is pivotal in illustrating that young stroke patients should always be evaluated for APS syndrome.[10,11] The remarkable youth of this patient at the time of diagnosis supports the view that this condition has a particular affinity for the younger population. As reported in a study, in young women, few studies have reported more than 14% of the cases of ischemic stroke in the young caused by this syndrome.[1,2] The cerebellar and cerebral hemispheres’ involvement in MRI scans is another classical finding seen in strokes associated with APS.[3]
The investigative details of this case, especially the lupus anticoagulant elevation, are characteristic of APS syndrome. Multiple studies have pointed out that lupus anticoagulants are a prothrombotic condition among the other antiphospholipid antibodies.[6,12] Other potential mimics, such as SLE and systemic lupus erythematosus, are also less likely because of the absence of other autoimmune antibodies.
The management strategy that was applied to this patient, including long-term anticoagulation with a vitamin K antagonist (warfarin), is in line with the appropriate management of thrombotic APS. Several large observational studies and meta-analyses have shown that vitamin K antagonists were more effective than antiplatelet drugs in preventing recurrent thrombotic episodes in patients with APS. The accompanying antiplatelet agents and statins, as in this case, are also a rational adjunct to the multifaceted problem of the pathophysiology of stroke due to APS.[11,13]
Conclusion
In conclusion, this case emphasizes the importance of investigating APS in young adults who have had an acute ischemic stroke, especially when there is considerable cerebrovascular involvement. A timely diagnosis and appropriate anticoagulant therapy are critical. Comprehensive laboratory testing, including antiphospholipid antibody evaluations, improves recovery prospects and establishes a firm diagnosis. A vitamin K antagonist was found to be effective for long-term anticoagulant therapy.
References
- Ekker MS, Boot EM, Singhal AB, et al. Epidemiology, aetiology, and management of ischaemic stroke in young adults. Lancet Neurol. 2018;17(9):790-801. doi:10.1016/S1474-4422(18)30233-3 PubMed | Crossref | Google Scholar
- Shkrobot S, Milevska-Vovchuk L, Duve K, Naumova L, Budarna O. A clinical case report: stroke in a young patient with systemic lupus erythematosus on the background of secondary antiphospholipid syndrome. Med Perspekt. 2022;27(4):259–263. doi:10.26641/2307-0404.2022.4.271243 Crossref | Google Scholar
- Chandrasekararan P, Mugundhan K. A study of ischemic stroke in young adults in tertiary care hospital in Salem. IAIM. 2020;7(9):12-18. A study of ischemic stroke in young adults in tertiary care hospital in Salem
- Anastasiadi A, Bott C, Kitterer D, et al. Primary antiphospholipid syndrome in the elderly: Four strokes and mechanical thrombectomies until the diagnosis – A case report. Brain Circ. 2024;10(2):184-187. 2024. doi:10.4103/bc.bc_67_23 PubMed | Crossref | Google Scholar
- Gonzalez-Salido J, Barron-Cervantes NM, Colado-Martinez J, et al. Ischemic Stroke as an Initial Manifestation of Antiphospholipid Syndrome in an Adolescent: A Case Report. Cureus. 2024;16(3):e55579. doi:10.7759/cureus.55579 PubMed | Crossref | Google Scholar
- Porey C, Jaiswal BK. Isolated intracranial hypertension without cerebral venous sinus thrombosis in APLA syndrome: an unique association. Int J Neurosci. 2024;134(12):1547-1550. doi:10.1080/00207454.2023.2273764 PubMed | Crossref | Google Scholar
- Neoh KK, Tang ASN, Looi I, Anita BM. Ischemic Stroke in a Young Patient with Nephrotic Syndrome and Antiphospholipid Syndrome. Case Rep Nephrol. 2020;2020:8828864. doi:10.1155/2020/8828864 PubMed | Crossref | Google Scholar
- Nakajima H, Tsuchiya T, Shimizu S, Suzuki H. Efficacy of mechanical thrombectomy for acute ischemic stroke in primary immune thrombocytopenia patient: Case report and literature review. Brain Hemorrhages. 2024;5(3):151-154. doi:10.1016/j.hest.2023.10.002 Crossref | Google Scholar
- Hamsho S, Alaswad M, Makhlouf Z, Alcheikh S. Septal atrial thrombosis as a primary presentation of antiphospholipid syndrome in a patient with ANA-negative systemic lupus erythematosus: a case report. Ann Med Surg (Lond). 2024;86(4):2189-2193. doi:10.1097/MS9.0000000000001668 PubMed | Crossref | Google Scholar
- Sarecka-Hujar B, Kopyta I. Antiphospholipid syndrome and its role in pediatric cerebrovascular diseases: A literature review. World J Clin Cases. 2020;8(10):1806-1817. doi:10.12998/wjcc.v8.i10.1806 PubMed | Crossref | Google Scholar
- Aneja J, Kuppili PP, Paul K, Panda S, Purohit A. Antiphospholipid syndrome presenting as treatment resistant bipolar disorder and thrombocytopenia in a young male. J Neuroimmunol. 2020;343:577238. doi:10.1016/j.jneuroim.2020.577238 PubMed | Crossref | Google Scholar
- Kiran GR, Shashivardhan J, Chandrasekhar P. Left Ventricular Thrombus: An Interesting Presentation of Primary Antiphospholipid Antibody Syndrome with a Mini-review of the Literature. J Cardiovasc Echogr. 2020;30(4):217-222. doi:10.4103/jcecho.jcecho_52_20 PubMed | Crossref | Google Scholar
- Ahammed T, Rasel M, Saha S, Istiak A, Chowdhury S. Primary antiphospholipid syndrome in a male presents with acute digital ischemia: Dramatic response to glucocorticoid. Clin Case Rep. 2024;12(4):e8749. doi:10.1002/ccr3.8749 PubMed | Crossref | Google Scholar
Acknowledgements
Not reported
Funding
None
Author Information
Corresponding Author:
Fatima Khurshid
Department of Radiation Oncology
Shifa International Hospital Ltd, Islamabad, Pakistan
Email: fatimakhurshid61@yahoo.com
Co-Authors:
Asif Islam
Department of Medicine & Rheumatology
Ali Fatima Hospital, Lahore, Pakistan
Umer Haider, Kinza Shahid Randhawa
PGR Medicine Department
Ali Fatima Hospital, Lahore, Pakistan
Memoona Khalood
Department of Radiology
Ali Fatima Hospital, Lahore, Pakistan
Authors Contributions
Asif Islam was responsible for the study concept and design. Umer Haider and Kinza Shahid Randhawa contributed to data collection. Fatima Khurshid handled the drafting of the work and manuscript write-up, while Memoona Khalood performed the final review.
Informed Consent
Informed consent was obtained from the patient.
Conflict of Interest Statement
None
Guarantor
The guarantor of this case report is Fatima Khurshid.
DOI
Cite this Article
Islam A, Haider U, Khurshid F, Randhawa KS, Khalood M. Primary Antiphospholipid Syndrome Presenting as a Stroke in Young Male. medtigo J Neurol Psychiatr. 2025;2(4):e3084242. doi:10.63096/medtigo3084242 Crossref









