Author Affiliations
Abstract
Background: Phlebitis, which is irritation of a blood vessel usually caused by intravenous (IV) catheterization, is a significant health problem worldwide with a higher predilection in hospital patients irrespective of their ward.
Aim: The aim of this study is to assess the proportion of hospitalized patients with phlebitis and to determine factors linked to it.
Methodology: A cross-sectional study was conducted over four weeks, enrolling 200 patients with peripheral venous cannulas inserted for 24 hours or longer. Data were collected using a structured questionnaire that included demographic information, underlying health conditions, and the presence of phlebitis. The prevalence was analyzed in relation to demographic variables and the causes of phlebitis.
Results: The overall prevalence of phlebitis was found to be 20%, with the highest incidence in the medical intensive care unit (ICU) (30%). Patients aged 31 to 45 years had the highest prevalence (25%), while mechanical trauma was identified as the primary cause (40%). The predominant management strategy involved the application of warm compresses, used for 70% of patients with phlebitis.
Conclusion: The findings highlight the need for improved monitoring and management strategies for phlebitis in hospitalized patients, especially in high-risk groups such as those in intensive care settings. Implementing standardized protocols, enhancing staff education, and fostering multidisciplinary collaboration can significantly reduce the incidence of phlebitis. Future research should focus on evaluating the effectiveness of targeted interventions to prevent this complication and improve patient outcomes related to intravenous therapy. This study underscores the importance of vigilance in intravenous catheter management to enhance patient safety in clinical environments.
Keywords
Phlebitis, Prevalence, Admitted patients, Intravenous therapy, Risk factors.
Introduction
Phlebitis, which is irritation of a blood vessel usually caused by IV catheterization, is a significant health problem worldwide, with a higher predilection in hospital patients irrespective of their ward.[1] This condition is due to mechanical irritation, chemical reactions, or infection and can cause discomfort, pain, and in some cases, dangerous complications. Long-term IV patients are especially vulnerable to this problem as catheter use precipitates inflammation of the vein walls.[2] Phlebitis not only jeopardizes patients’ health but also delays lengths of stay and increases already skyrocketing costs. It is important to estimate and manage the risk factors of phlebitis to promote the consideration of enhanced patient outcomes and safer hospitals.[3]
Venous inflammation is a widespread occurrence among patients in healthcare institutions in which vein catheterization takes place for the administration of drugs, interference with hydration, and supportive feeding.[4] The incidence of phlebitis depends on the type of IV catheter, frequency of catheter replacement, and certain medications given.[5] Therefore, the analysis of phlebitis is essential to the overhaul of an aspect of health care that is preventable.[6]
Some research shows that deep vein thrombosis is usually underdiagnosed, and many patients are asymptomatic, or their symptoms are not discovered until later on. Possible causes of the rates of phlebitis include policies and practices in the healthcare facility and nursing expertise, apart from infection control.[7] The issue is not isolated to some patient populations; phlebitis can affect the patient’s age and acuity. Therefore, an investigation into the possible antecedent causes of phlebitis in the various wards may produce results that will inform healthcare organizations on how best to prevent the occurrence of phlebitis.[8]
Phlebitis has complications of discomfort, including minor types to the most severe conditions such as bloodstream infections and deep vein thrombosis. Indicators included erythema, pain on palpation, an increase in temperature, and oedema of the skin around the point of catheterization.[9] If left untreated, phlebitis can worsen and can result in the formation of thrombophlebitis, increasing the chance of infection and affecting patient outcomes.[10] Hence, it is very important to address and control the uptake of phlebitis if improved and safer delivery of care is to be realized in hospitals.[11]
Methodology
This research used a cross-sectional study design to determine the incidence of phlebitis among hospitalized patients. The present study was conducted in a tertiary care hospital Swat. The target population in this study comprised all the admitted patients in the four mentioned wards (Medical ICU, medical ward, orthopedic ward, surgical ward). Patients admitted to any of the mentioned wards of the tertiary care hospital during the study period, Patients who had a peripheral intravenous catheter inserted for medication administration, fluids, or other medical purposes, were included. The sample size for this study was determined using the OpenEpi calculator. With a statistical power of 80% and a 95% confidence interval, the calculated sample size was 200 patients. Data collection employed a convenience sampling method, allowing for the efficient selection of participants who met the inclusion criteria.
Data Collection:
The research instrument consisted of a structured questionnaire, validated (Content validity index (CVI) = 0.90) and Reliable (Cronbach’s alpha (CA) 0.84). Data were gathered through structured questionnaires, bedside assessments, patient interviews, and site observations. Key demographic, clinical, and phlebitis-related information was recorded, with phlebitis severity graded using the visual infusion phlebitis (VIP) scale.
Quality assurance measures, including a pilot study and supervision by clinical staff, ensured data reliability. Data collection took place over four weeks, with all information securely stored to maintain confidentiality. This systematic approach provided a solid basis for analyzing phlebitis prevalence and associated factors.
Data Analysis:
Data were analyzed using the statistical package for social sciences (SPSS) version 27, a statistical software package that facilitated comprehensive data analysis. All variables, including demographic and clinical factors, were presented as percentages. A Chi Square statistical test was applied to assess significance, with a p-value of less than 0.05 indicating statistical significance.
Ethical Consecration:
Ethical approval was taken from the institutional review board (IRB) committee SGTH, Swat, Pakistan (Ref No SGTH/ IRB/25/03). All respondents’ written consent was obtained after explaining the purpose of the study and their rights. Prestige and confidentiality were observed throughout the data gathering and analysis process. Consent was granted, and participants were free to make decisions on a voluntary basis and even withdraw at their discretion from the study. All data were collected innocuously as we did not involve any manipulation or dishonest measures to report our findings.
Results
The demographic information of the 200 participants from the study. The results for age showed that the highest percentage of patients were within the 31-45 years of age, and there was an equal distribution between male and female patients, with each being 50%. (Table 1)
| Demographic Variable | Frequency (n) | Percentage (%) |
| Age (Years) | ||
| 18-30 | 40 | 20 |
| 31-45 | 60 | 30 |
| 46-60 | 50 | 25 |
| 61 and above | 50 | 25 |
| Gender | ||
| Male | 100 | 50 |
| Female | 100 | 50 |
| Ward type | ||
| Medical ICU | 50 | 25 |
| Medical ward | 70 | 35 |
| Orthopedic ward | 40 | 20 |
| Surgical ward | 40 | 20 |
| Underlying conditions | ||
| Diabetes mellitus | 40 | 20 |
| Hypertension | 30 | 15 |
| Smoking | 20 | 10 |
| No underlying condition | 110 | 55 |
Table 1: Demographic characteristics of study participants
The incidence of phlebitis among the participants of the study was based on demographic factors. In the present study, the overall rate of Phlebitis was 20%. (Table 2)
| Demographic variable | Patients with phlebitis (n) | Prevalence (%) |
| Age (Years) | ||
| 18-30 | 5 | 12.5 |
| 31-45 | 15 | 25 |
| 46-60 | 10 | 20 |
| 61 and above | 10 | 20 |
| Gender | ||
| Male | 25 | 25 |
| Female | 15 | 15 |
| Ward type | ||
| Medical ICU | 15 | 30 |
| Medical ward | 20 | 28.57 |
| Orthopedic ward | 5 | 12.5 |
| Surgical ward | 5 | 12.5 |
Table 2: Prevalence of phlebitis by demographic characteristics
The major causes of the formation of phlebitis among the involved patients. The most common cause of mechanical trauma was seen to be intravenous cannulas; they comprised 40 percent of all cases. (Table 3)
| Reason for phlebitis | Frequency (n) | Percentage (%) |
| Mechanical trauma | 20 | 40 |
| Chemical irritation | 15 | 30 |
| Infection | 10 | 20 |
| Unknown causes | 5 | 10 |
Table 3: Reasons for phlebitis development among affected patients
The approaches to the treatment and management of patients diagnosed with phlebitis. For each of the assessed symptoms, most patients (70%) received warm compresses that help eliminate discomfort and reduce inflammation as well.
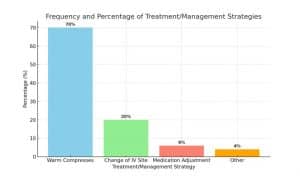
Figure 1: Treatment and management of phlebitis
Discussion
Hence, the results of this study on the frequency of phlebitis among hospitalized patients can provide knowledge about patients’ characteristics and the risk factors for phlebitis – a typical complication that may occur when patients receive intravenous catheterization. Given an overall prevalence rate of 20%, the results are consistent with those highlighted in prior literature that have highlighted moderate variability in the prevalence of the disorder across different study subject groups and clinical contexts. The findings indicate that some patients appear to be more susceptible to phlebitis than others, and that age and gender are primary factors that need to be addressed.[12]
On the issue of age distribution, the study showed that subjects between 31 and 45 years had the highest incidence of phlebitis at 25 percent. This discovery is useful as this age group has multiple comorbidities and may necessitate long IV courses.[13] Phlebitis is dependent on catheterization time; therefore, this age group should be observed closely for any signs of inflammation or complications of IV access.[14] Moreover, the genders of the participants are equal, which indicates that both males and females must be monitored closely, as no bias was acknowledged. [15]
The ward type also contributed to the phlebitis proneness, but at a much lower measure compared to the catheter-related factor, with the Medical ICU having a 30% prevalence rate. This finding highlights the modulation of critically ill patients with a variety of comorbidities, with frequently compromised skin integrity, who may require extensive intravenous access.[16] The findings reveal that critical care delineates the need for strict aseptic techniques and periodic IS observation to decrease phlebitis incidence.[17] It is also noteworthy that the rate in medical wards was somewhat higher than in surgical and orthopedic ones, and this could be due to the type of patients’ pathology and perhaps to the more frequent handling of catheters in those wards.[18]
Surveying the core antecedent conditions, most respondents had no diagnosed medical illnesses; however, a substantial proportion of patients had diagnosed diabetes mellitus and hypertension. On the same note, diabetes is one of those diseases that weaken the body’s immune system and compromise circulation, thus allowing infection and the development of diseases such as phlebitis. Described relationship underlines the necessity of studying proper patient histories in order to identify individuals at increased risk.[19] The strategy that should be utilized by the healthcare teams is patient education, which means that they should educate the patients on the signs and symptoms of phlebitis so that, in the unlikely event that they occur, they report early to avoid worse results.[20]
Mechanical trauma was the most common condition contributing to phlebitis in the patients that were studied by the authors of the manuscript at 40%. This calls for better measures when performing catheterization and care on the patients. Peripherally inserted intravenous tools, such as catheters, are bent on insertion or are stabilized and handled in particular ways; staff education on the same helps to address the mechanical irritation that may harm the patient.[21] Furthermore, ongoing training and clinical supervision may contribute to the overall reduction in the occurrence of phlebitis, especially in high-risk clinical groups.[22]
The study showed that the management strategies that were used included warm compress application to the affected patient, which yielded a 70% success rate on the phlebitis-affected patients. Although this approach offers an anti-inflammatory remedy and pain control for the manifestation of phlebitis, this isn’t the only solution that can be exercised; it might prove useful if standard of care measures for prevention and treatment of the condition are developed.[23] This could include conducting APRs of intravenous sites and setting up a protocol for the nurses to handle phlebitis to ensure quality care is being delivered in different care units by different caregivers.[24]
From these studies, furthermore, urges the need to be more proactive in preventing phlebitis, especially in the ICU. Healthcare institutions should perhaps liaise and establish standard clinical practice protocols that incorporate frequent assessment and evaluation of IV access sites, especially for high-risk patients who are perhaps due to age or comorbidity.[25] Furthermore, awareness creation concerning personal safety among healthcare staff will greatly enhance the rate of complications among patients receiving IV therapy.[26]
Thus, the present work offers useful empirical findings for understanding the incidence and risk determinants of phlebitis among hospitalized patients. These demographic findings, in combination with the most common etiologies and management approaches demonstrated, emphasize the necessity for improved surveillance and individualized preventive measures regarding the incidence of phlebitis. Concerning the complexity of healthcare management, patient safety and proper control of possible IV therapy complications will remain the focal points in the ongoing process of developing healthcare delivery and increasing good patient outcomes.
Recommendations: Based on the findings of this study, the following recommendations are proposed to enhance the management and prevention of phlebitis among hospitalized patients:
Implementation of Standardized Protocols: Intravenous catheters for healthcare facilities should recommend universal approaches to catheter insertion, management, and removal. Such practices should cover issues related to the selection of a site for a catheter, proper use of sterilization procedures, and monitoring of points of intravenous access to reduce cases of phlebitis.
Staff Training and Education: Healthcare workers need to have orientation seminars where issues concerning catheter care and identification of catheter-associated phlebitis are discussed. Thus, educational programs could pay more attention to the most significant risks and, in this way, facilitate staff adherence to the protocols, which could decrease the complication rate.
Routine Assessment and Monitoring: Set up the basics of evaluating patients with IV catheters at specific intervals, preferably more frequent intervals, especially in high-risk units like MICU. This should include a daily assessment of the insertion site for any signs of inflammation, and then intervene appropriately when it is necessary.
Patient Education: Inform patients and their families of ameliorated risks related to intravenous therapy, which include phlebitis and its indicators. When a patient is given information on when to come with concerns, then complications can be detected early and treated.
Research on Intervention Strategies: More research should be conducted to understand more about recommended intervention approaches that can be used to prevent phlebitis among such vulnerable groups of patients. Research may isolate the use of catheter materials, techniques for catheter placement, and the arrangement of the patient’s position on how it affects phlebitis.
Multidisciplinary Collaboration: GNM-General nurses, medical doctors, and pharmacists should form a team to enhance the formulation of a coordinated care delivery plan for patients on IV therapy. I also realized that such an approach of forming a team of individuals involved in the care of a patient can enhance coordination so that all the aspects of a patient’s treatment are covered.
Use of Technology: Discuss the implementation of, for instance, an electronic health record system and alert systems that will point out patients with a higher risk of phlebitis given their medical histories and current management plans. Other ways to improve monitoring involve coming up with reminders for checking IV sites.
Data Collection and Surveillance: Implement a standing process to monitor and collect data regarding the incidence of phlebitis in healthcare delivery institutions. Consequently, identifying trends through ongoing surveillance of unsafe conditions will afford HS oversight with valuable information that will help inform policy and practice changes toward enhancing patient safety.
Conclusion
In conclusion, the findings of this research will be useful to clinicians and policymakers wanting to identify areas of practice that could be modified to decrease the occurrence of phlebitis in hospitalized patients. As always, the elevation of standards in education, compliance with set best practices in intravenous therapy, and safe patient monitoring should improve patients’ safety and health. Additional studies should be dedicated to the establishment and assessment of specific strategies to prevent such causes of phlebitis and provide an addition to existing knowledge used in intravenous-related practices within clinical environments.
References
- Gupta P, Vardhan N, Ravindran B, Durga K, Marthathi S. Chondromyxoid fibroma of the metatarsal head: A rare case report. J Clin Diagn Res. 2024;10(6):CR01-03. doi:10.7860/JCDR/2024/67732.19128 Crossref | Google Scholar
- Lezama J. Internal Medicine Learning Using 1, 2, 3 Methodology. eBook. Springer Cham publishing; 2024. Internal Medicine Learning A to Z and 1, 2, 3: A High Reliability Approach to Clinical Knowledge and Standardized Testing Success | SpringerLink
- Jain N, Avanthika C, Singh A, et al. Deep Vein Thrombosis in Intravenous Drug Users: An Invisible Global Health Burden. 2021;13(10):e18457. doi:10.7759/cureus.18457 PubMed | Crossref | Google Scholar
- Lulie M, Tadesse A, Tsegaye T, Yesuf T, Silamsaw M. Incidence of peripheral intravenous catheter phlebitis and its associated factors among patients admitted to University of Gondar hospital, Northwest Ethiopia: a prospective, observational study. Thromb J. 2021;19(1):48. doi:10.1186/s12959-021-00301-x PubMed | Crossref | Google Scholar
- Al-Khafaji RA, Schierbeck L. Deep Venous Thrombosis in a Patient with a Moderate Pretest Probability and a Negative D-Dimer Test: A Review of the Diagnostic Algorithms. J Blood Med. 2020;11:173-184. doi:10.2147/JBM.S244773
PubMed | Crossref | Google Scholar - Wenger N, Sebastian T, Engelberger RP, Kucher N, Spirk D. Pulmonary embolism and deep vein thrombosis: Similar but different. Thromb Res. 2021;206:88-98. doi:10.1016/j.thromres.2021.08.015 PubMed | Crossref | Google Scholar
- Sharifpour M, Bittner EA. Critical Care of the Vascular Surgery Patient. Anesthesiol Clin. 2022;40(4):775-790. doi:10.1016/j.anclin.2022.08.017 PubMed | Crossref | Google Scholar
- Wolf K, Hu H, Isaji T, Dardik A. Molecular identity of arteries, veins, and lymphatics. J Vasc Surg. 2019;69(1):253-262. doi:10.1016/j.jvs.2018.06.195 PubMed | Crossref | Google Scholar
- Gunasundram S, Tan M, Lim KZH, Loh VMP. Reducing the incidence of phlebitis in medical adult inpatients with peripheral venous catheter care bundle: a best practice implementation project. JBI Evid Implement. 2021;19(1):68-83. doi:10.1097/XEB.0000000000000245 PubMed | Crossref | Google Scholar
- Yasuda H, Yamamoto R, Hayashi Y, et al. Occurrence and incidence rate of peripheral intravascular catheter-related phlebitis and complications in critically ill patients: a prospective cohort study (AMOR-VENUS study). J Intensive Care. 2021;9(1):3. doi:10.1186/s40560-020-00518-4 PubMed | Crossref | Google Scholar
- Sari I, Ginting C, Nasution SW. Analysis of the relationship between nurses’ knowledge of infusion therapy with the incidence of phlebitis and patient comfort. J La Medihealtico. 2024;5(1):185-203. doi:10.37899/journallamedihealtico.v5i1.1069 Crossref | Google Scholar
- Tetali S, Fricker A, Domburg YA, Roy I. Intelligent biomaterials for cardiovascular applications. Curr Opin Biomed Eng. 2023;28:100474. doi:10.1016/j.cobme.2023.100474 Crossref
- Monchka BA, Leung CK, Nickel NC, et al. The effect of disease co-occurrence measurement on multimorbidity networks: a population-based study. BMC Med Res Methodol. 2022;22:165. doi:10.1186/s12874-022-01607-8
PubMed | Crossref | Google Scholar - Danielle RCS, Débora DM, Alessandra NLP, et al. Correlating COVID-19 severity with biomarker profiles and patient prognosis. Sci Rep. 2024;14(1):22353. doi:10.1038/s41598-024-71951-w PubMed | Crossref | Google Scholar
- Del Barco AW. Implementation of a phlebitis prevention bundle on a neurotrauma critical care unit. Degree thesis. University of Maryland; 2022. Dissertation Title Page Template
- Gauci M. Developing a venous access guideline in Malta: a modified delphi study. Master’s thesis. University of Malta; 2022. edu.mt/library/oar/bitstream/123456789/110101/1/22MSNR13_Maria_Gauci.pdf
- Marsh N, Larsen EN, Ullman AJ, et al. Peripheral intravenous catheter infection and failure: A systematic review and meta-analysis. Int J Nurs Stud. 2024;151:104673. doi:10.1016/j.ijnurstu.2023.104673 PubMed | Crossref | Google Scholar
- Lee MR. Peripheral intravenous catheter compliance in the acute care setting. Montana State University; 2024:1-48. Peripheral Intravenous Catheter Compliance in the Acute Care Setting
- Daryabor G, Atashzar MR, Kabelitz D, Meri S, Kalantar K. The Effects of Type 2 Diabetes Mellitus on Organ Metabolism and the Immune System. Front Immunol. 2020;11:1582. doi:10.3389/fimmu.2020.01582
PubMed | Crossref | Google Scholar - Galang H, Hubbard-Wright C, Hahn DS, et al. A Randomized Trial Comparing Outcomes of 3 Types of Peripheral Intravenous Catheters. J Nurs Care Qual. 2020;35(1):6-12. doi:10.1097/NCQ.0000000000000421
PubMed | Crossref | Google Scholar - Orhurhu V, Chu R, Xie K, et al. Management of Lower Extremity Pain from Chronic Venous Insufficiency: A Comprehensive Review. Cardiol Ther. 2021;10(1):111-140. doi:10.1007/s40119-021-00213-x
PubMed | Crossref | Google Scholar - Cicolini G, Comparcini D, Simonetti V, Maria Papappicco CA, Unsworth J, Tomietto M. Nurses’ knowledge and self-assessment of their clinical experiences of intraosseous access: A multicentre cross-sectional study. Int Emerg Nurs. 2023;69:101314. doi:10.1016/j.ienj.2023.101314 PubMed | Crossref | Google Scholar
- Karunarathna I, Alvis K, Gunasena P, et al. Perioperative and ICU care for COPD patients: enhancing outcomes through multidisciplinary approaches. 2024:1-11. doi:10.13140/RG.2.2.17651.54566 Google Scholar
- Cottrill KN. Implementation of an amiodarone infusion nurse practice guideline to reduce the incidence of phlebitis: a quality improvement project. Degree thesis. West Virginia University; 2022. “Implementation of an Amiodarone Infusion Nurse Practice Guideline to R” by Kristen N. Cottrill
Acknowledgments
Not reported
Funding
None
Author Information
Corresponding Author:
Khanzada
Department of Nursing
Nutrition Ward DHQ MTI D.I Khan, Pakistan
Email: khanzada1743@gmail.com
Co-Authors:
Rahila Gul, BiBi Amina
Department of Nursing
Regional Blood Center D.I Khan, Pakistan
Saba Farid
Department of Nursing
Female Orthopedic Ward DHQ MTI D.I Khan, Pakistan
Authors Contributions
Khanzada was responsible for data collection and analysis. Rahila Gul handled data analysis. Saba Farid and BiBi Amina contributed to data collection.
Ethical Approval
Ethical approval was taken from the IRB committee SGTH, Swat, Pakistan (Ref No SGTH/ IRB/25/03). All respondents’ written consent was obtained from them after explaining the purpose of the study and their rights.
Conflict of Interest Statement
None
Guarantor
None
DOI
Cite this Article
Khanzada, Rahila G, Saba F, BiBi A. Prevalence and Risk Factors of Phlebitis Among Hospitalized Patients in Various Wards of a Tertiary Care Hospital in Swat, Pakistan. medtigo J Med. 2025;3(1):e30623126. doi:10.63096/medtigo30623126 Crossref






