Author Affiliations
Abstract
Confluent and reticulated papillomatosis (CRP) is a rare and often underdiagnosed disorder of keratinization that poses a significant clinical challenge due to its resemblance to more common pigmentary conditions, particularly acanthosis nigricans. Although first described more than 60 years ago, the pathogenesis of CRP remains incompletely understood. Recent microbiologic studies have identified an association between CRP and Dietzia species (family Dietziaceae; suborder Corynebacterineae; order Actinomycetales), implicating a potential bacterial trigger and providing a compelling explanation for the marked clinical response to antibiotic therapy. This emerging link represents a shift in understanding CRP from a purely keratinization disorder to a condition with a possible infectious component. We report a 15-year-old female with a one-year history of pruritic, brown hyperkeratotic papules on the abdomen and thorax, unresponsive to antifungals and topical corticosteroids. Histopathology revealed orthokeratosis, irregular acanthosis, papillomatosis with digitiform projections, compact hyperkeratosis, focal parakeratosis, and mild basal hyperpigmentation without atypia. Differential diagnoses included Cushing’s disease, Pityrosporum infection, and cutaneous amyloidosis. A skin biopsy confirmed CRP, which typically presents as verrucous or hyperkeratotic papules coalescing into plaques with a peripheral reticulated pattern. While oral minocycline is the traditional treatment, azithromycin offers a safer, effective alternative. Emerging evidence links Dietzia species to CRP, highlighting the importance of recognizing this association for accurate diagnosis and optimized antimicrobial therapy.
Keywords
Confluent and reticulated papillomatosis, Microscopic examinations, keratinization, skin biopsy, and minocycline.
Introduction
CRP is a condition caused by disorganized keratinization. This disease was originally described by Gougerot and Carteaud and is also known as Gougerot–Carteaud syndrome (LeeSW). Confluent and reticulated Gougerot–Carteaud papillomatosis is an uncommon dermatological condition that affects adolescents, especially young dark-skinned women. It presents asymptomatic pigmented macules with a papillomatous texture that merge to form reticulated plaques located on the neck and intertriginous areas. The etiology of this condition remains unclear; however, abnormal keratinization has been implicated, and some cases have been associated with Malassezia species. The disease typically follows a chronic course characterized by periods of remission and exacerbation.[1-4]
CRP has been described in different geographic areas and regions. Its frequency is higher in white individuals. The Mayo Clinic conducted a study between 1972 and 2003 with 39 patients diagnosed with confluent and reticulated papillomatosis, and determined that the average age of onset was 15 years, with a range of 8 to 32 years and a higher incidence in males, with a ratio of 1.4:1. A Japanese study obtained similar results, with an average age of 17 years, a range of 3 to 30 years, and a slightly higher incidence in males. A study from Singapore reported an average onset age of 29 years, with a range of 16 to 55 years and a higher incidence in males, with a ratio of 2.6:1.[5,6]
CRP is a rare dermatosis with an incompletely understood pathogenesis, in which genetic predisposition and abnormal keratinization have been proposed as contributing factors. The presence of consanguinity in the patient’s family may further support a potential genetic influence in the development of this condition. CRP presents significant diagnostic and therapeutic challenges due to its clinical overlap with other pigmentary disorders and the absence of standardized treatment guidelines, underscoring the need for continued investigation into its underlying mechanisms.[7,8]
Although multiple therapeutic approaches have been attempted with variable success, no definitive treatment has been established. Nevertheless, several studies have reported favorable outcomes with oral minocycline, often achieving sustained remission with no recurrence after six months of follow-up. Other antibacterial agents shown to be effective include fusidic acid (1000 mg daily), clarithromycin (500 mg daily), erythromycin (1000 mg daily), and tetracycline (James).[8,9]
Case Presentation
We present the case of a 15-year-old female presenting with a one-year history of pruritic, dark brown confluent papules affecting the thorax and abdomen, refractory to irregular treatment with fluconazole and topical betamethasone. Clinical and histopathological findings were consistent with CRP. Laboratory evaluation revealed elevated adrenocorticotropic hormone (ACTH) levels, raising the possibility of an underlying endocrine abnormality and prompting consideration of an association with Cushing’s disease, a relationship that has been infrequently reported in the literature. Additionally, increased serum IgE levels may reflect an underlying inflammatory or atopic predisposition, while vitamin D deficiency, commonly observed in chronic inflammatory and keratinization disorders, may contribute to disease persistence and impaired epidermal differentiation. Although these abnormalities are not specific, their coexistence highlights the complexity of CRP and the importance of a comprehensive systemic evaluation.
This case underscores the rarity of CRP, the challenges involved in establishing an accurate diagnosis, and the need to consider endocrine and metabolic factors in refractory presentations. Greater awareness of these associations may facilitate earlier recognition and more individualized management of this uncommon condition (Davis).

Figure 1: First day attended at Sanus Medical Offices
Physical examination:
Vital signs:
- Heart rate: 70 beats per minute
- Respiratory rate: 17 breaths per minute
- Oxygen saturation: 96%
- Axillary temperature: 2 °C
Anthropometric measurements:
- Height: 151 cm
- Weight: 43 kg
- Body mass index (BMI): 85 (Malnutrition)
Level of consciousness:
- Glasgow coma scale: 15/15
- Level of consciousness: Patient awake
Skin and appendages:
- Elasticity and turgor preserved, well hydrated. Capillary refill: 2 seconds.
- Morphology: papules (elevated lesions). Asymptomatic.
- Coloration: Brown, irregular, poorly defined borders, brownish and erythematous, with slight lacerations.
- Texture: Hyperkeratotic
- Distribution: Central confluent pattern with peripheral Located on the abdomen and anterior thorax, with lightly pruritic signs and dermographism around the lesions.
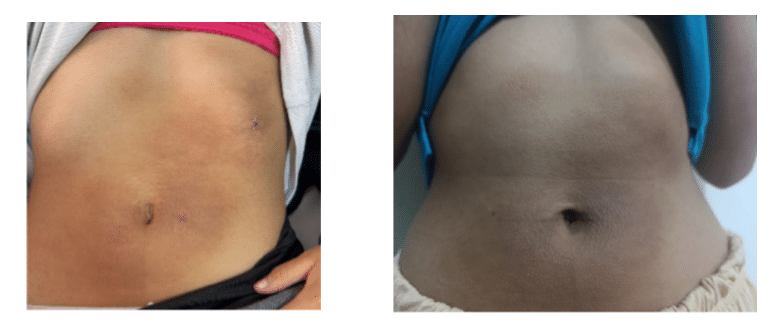
Figure 2: Patient condition one year ago while on corticosteroid treatment, and the other image shows the first day of follow-up at Sanus Medical Offices
Regional physical examination:
- Cranium: Head:
- Neck: Mobile, no lymphadenopathy.
- Thorax: Symmetric; heart with regular rhythm; lungs without adventitious
- Abdomen: Symmetric; non-tender on palpation; bowel sounds
- Genital region: Not
- Extremities: Turgor and elasticity preserved; Daniels scale 5/5. Reflexes

Figure 3: Patient attending follow-up after biopsy at Sanus Medical Offices
Laboratory tests:
- Cortisol AM: 4 µg/dL (6.2–19.49)
- Adrenocorticotropic hormone (ACTH): 00 pg/mL (0–46)
- Total IgE (Immunoglobulin E): 1 IU/mL (0–87)
- Total vitamin D 25 OH (D3 + D2): 33 ng/mL
Histopathology:
- Specimen: Abdominal skin: Skin from the edge of the umbilicus and skin from the left costal
- Procedure: Biopsy
- Histological type: Findings consistent with confluent and reticulated papillomatosis (Gougerot–Carteaud)
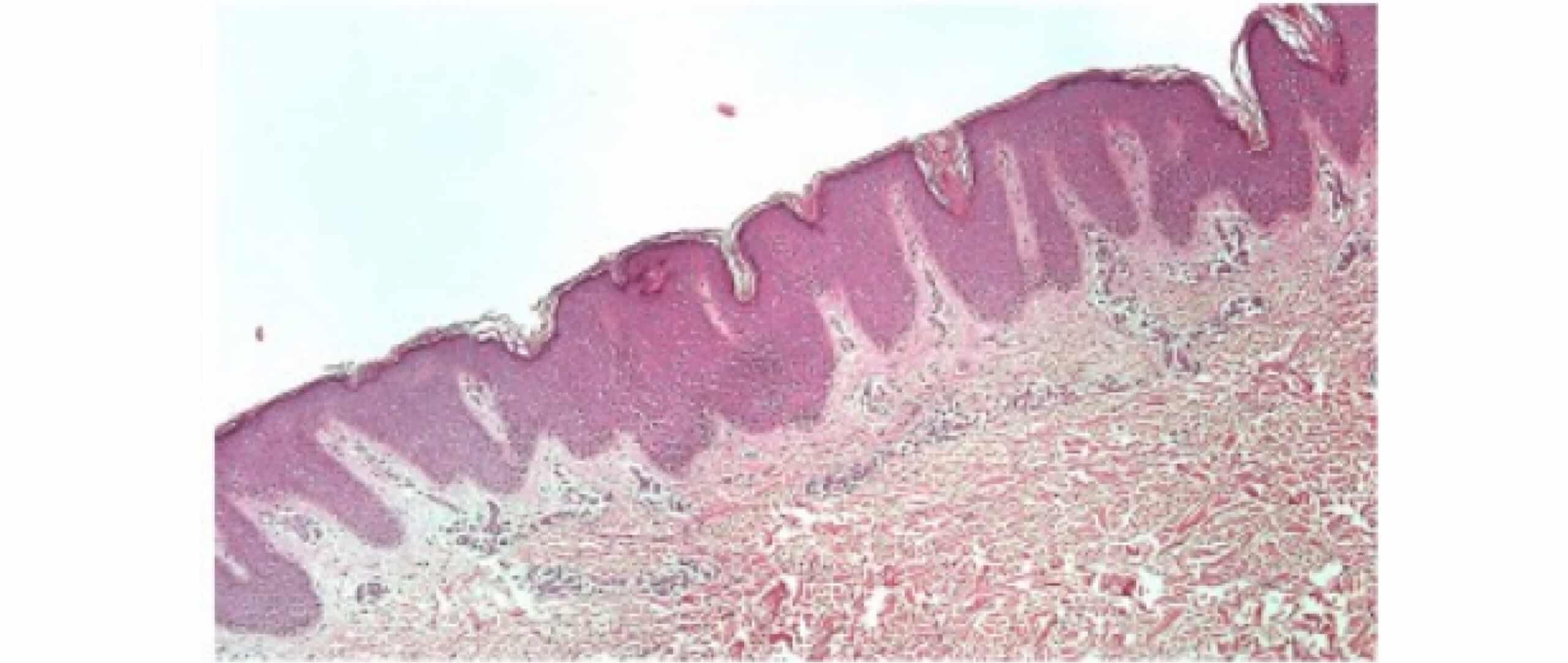
Figure 4: Histopathological result of biopsy samples, responsible: Cristian Galarza S.
Discussion
CRP is a poorly recognized dermatological disorder of uncertain etiology. Although its precise pathogenesis is not yet fully understood, it is hypothesized to result from a defect in epidermal keratinization, which may be either genetic or acquired. Furthermore, a potential association with Malassezia furfur has been described, either because fungal colonization induces keratinization abnormalities or due to an atypical host immune response.[1-3]
This theory is supported by the characteristic distribution of the lesions; however, the fact that it does not improve with antifungals, as in our case, casts doubt on its validity. Associations with endocrine disorders (obesity, type 2 diabetes mellitus, hirsutism, Cushing’s syndrome, or thyroid disease), photosensitivity, and cutaneous amyloidosis have also been described.
We report two cases of confluent and reticulated papillomatosis. Case 1 involved a 24-year-old man with a six-month history of skin eruptions, and case 2 involved a 19-year-old woman with a three-day history of the condition. Both patients exhibited dark brown reticular papules with mild keratosis and infiltration, extending from the trunk to the neck and upper arms. Direct optical microscopy did not detect fungi, and histopathological examinations confirmed hyperkeratosis, acanthosis, papillomatosis, and mild infiltration of small round cells. Therefore, both patients were diagnosed with confluent and reticulated papillomatosis and neither had diabetes nor thyroid dysfunction. In case 1, cefdinir was effective, while in case 2, minocycline hydrochloride and ketoconazole were effective.[6]
Conclusion
CRP is a rare and frequently underdiagnosed dermatological disorder, where accurate clinical and histopathological recognition is essential for effective therapeutic management. Although its etiology remains uncertain, evidence indicates that keratinization abnormalities play a central role, with potential contributions from microorganisms such as Dietzia spp. or Malassezia furfur, as well as possible associations with endocrine disorders. The presented case highlights the importance of considering CRP in the differential diagnosis of hyperkeratotic dermatoses that do not respond to conventional antifungal or corticosteroid treatments. Confirmation via skin biopsy is essential for establishing a definitive diagnosis. Regarding treatment, minocycline remains the drug of choice due to its efficacy and dual antibacterial and anti-inflammatory action. However, azithromycin emerges as a promising alternative, particularly because of its better tolerability and lower incidence of adverse effects. Continued research is needed to elucidate the underlying pathophysiological mechanisms, the potential genetic influence, and the response to new therapeutic regimens, in order to optimize clinical management of this disease. Long-term follow-up and patient education are essential to prevent recurrences and improve quality of life.
References
- Angeli-Besson C, Koeppel MC, Jacquet P, Andrac L, Sayag J. Confluent and reticulated papillomatosis (Gougerot-Carteaud) treated with tetracyclines. Int J Dermatol. 1995;34(8):567-569. doi:10.1111/j.1365-4362.1995.tb02956.x
PubMed | Crossref | Google Scholar - Ginarte M, Fabeiro JM, Toribio J. Confluent and reticulated papillomatosis (Gougerot-Carteaud) successfully treated with tacalcitol. J Dermatolog Treat. 2002;13(1):27-30. doi:10.1080/09546630252775216
PubMed | Crossref | Google Scholar - Bowman PH, Davis LS. Confluent and reticulated papillomatosis: response to tazarotene. J Am Acad Dermatol. 2003;48(5 Suppl):S80-81. doi:10.1067/mjd.2003.155
PubMed | Crossref | Google Scholar - Errichetti E, Maione V, Stinco G. Dermatoscopy of confluent and reticulated papillomatosis (Gougerot-Carteaud syndrome). J Dtsch Dermatol Ges. 2017;15(8):836-838. doi:10.1111/ddg.13259
PubMed | Crossref | Google Scholar - Henderson Berg MH, Pehr K. Familial Confluent and Reticulated Papillomatosis in 2 Kindreds Including 3 Generations. J Cutan Med Surg. 2018;22(3):330-332. doi:10.1177/1203475417738968
PubMed | Crossref | Google Scholar - Lee SW, Loo CH, Tan WC. Confluent and reticulated papillomatosis: Case series of 3 patients from Kedah, Malaysia and literature review. Med J Malaysia. 2018;73(5):338-339.
Confluent and reticulated papillomatosis: Case series of 3 patients from Kedah, Malaysia and litera… - Le C, Bedocs PM. Confluent and Reticulated Papillomatosis. eBook. StatPearls Publishing; 2023.
Confluent and Reticulated Papillomatosis - Paller AS, Mancini AJ. Paller and Mancini – Hurwitz Clinical Pediatric Dermatology. 6th Edition. Elsevier; 2021.
Paller and Mancini – Hurwitz Clinical Pediatric Dermatology - Scheinfeld N. Confluent and reticulated papillomatosis: a review of the literature. Am J Clin Dermatol. 2006;7(5):305-313. doi:10.2165/00128071-200607050-00004
PubMed | Crossref | Google Scholar
Acknowledgments
We thank the medical staff at Sanus Medical Offices in Loja for allowing us to review and study the patient’s medical history, and Dr. Cristian Galarza, internist, diabetologist, and research faculty member of the Medicine program, for reviewing the manuscript.
Funding
The authors declare that no financial support or funding was received for the conduct of this study.
Author Information
Corresponding Author:
Cristian Alfonso Galarza Sánchez
Department of Internal Medicine
Clínica Abendaño, Loja, Ecuador
Email: cristiangalarzasanchez@gmail.com
Co-Authors:
Yulissa Michelle Chocho Gutiérrez
Department of General Medicine
Clínica Sanus, Ecuador
Marjorie Salome Cevallos Esparza
General Practitioner (Hospital Functions)
Solca Hospital, Loja, Ecuador
Joel Asdrúbal Rodríguez Gutiérrez
Department of Family Medicine
Mexican Institute of Social Security (IMSS, México)
Carlos Fernando Chuchuca Pardo
General Practitioner (Hospital Functions)
José Carrasco Arteaga Specialty Hospital, Ecuador
Wilman Roberto Uchuari Lalangui
General Practitioner
Clínica Sanus, Ecuador
Authors Contributions
Yulissa Michelle Chocho Gutiérrez participated in the clinical care of the patient, data collection, and initial drafting of the manuscript. Cristian Alfonso Galarza Sánchez contributed to the study conception, clinical analysis of the case, critical revision of the intellectual content, and approval of the final version. Marjorie Salome Cevallos Esparza collaborated in the collection of clinical information, literature review, and support in manuscript writing. Joel Asdrúbal Rodríguez Gutiérrez performed academic supervision, methodological review, and final manuscript editing. Carlos Fernando Chuchuca Pardo participated in the clinical evaluation of the patient and organization of the medical information. Wilman Roberto Uchuari Lalangui collaborated in clinical care, patient follow-up, and manuscript review. All authors read and approved the final version of the manuscript and take responsibility for its content.
Informed Consent
Written informed consent was obtained from the patient and/or the patient’s legal guardian for the publication of this case and the accompanying clinical images, ensuring anonymity.
Conflict of Interest Statement
The authors declare no conflicts of interest.
Guarantor
The guarantor of this case report is DR. CRISTIAN GALARZA.
DOI
Cite this Article
Gutiérrez YMC, Sánchez CAG, Esparza MSC, Gutiérrez JAR, Pardo CFC, Lalangui WRU. Irregular Brown Lesions With Poorly Defined Borders in an Asymptomatic 15-Year-Old Patient. medtigo J Med. 2025;3(4):e3062349. doi:10.63096/medtigo3062349 Crossref









