Author Affiliations
Abstract
Low back pain (LBP) has the highest prevalence globally among musculoskeletal conditions and is the leading cause of disability worldwide. A strong positive association between Modic type I change and LBP has been reported in most studies, but the prevalence varies greatly. There is no standard treatment protocol for Modic type I change at present. Intradiscal PRP injection is found to be effective in degenerative spinal disease in terms of improving pain and functional status. This study assessed the effect of intradiscal PRP (Platelet-rich plasma) in type I Modic change-associated LBP and the change of Modic type 1 on magnetic resonance imaging (MRI). PRP was injected intradiscally at the L4/5 disc under intermittent fluoroscopy. After 6 months, an MRI of the lumbar spine was carried out to see the changes in Modic type I. Assessment of pain by visual analogue scale (VAS) and disability by Roland‐Morris disability questionnaire (RMDQ) was done at different time intervals (pre-injection and post-injection at 1 week, 1 month, 3 months, 6 months, and 12 months). Quality of life was measured by the 12-item short form health survey (SF-12) before injection and after injection of PRP (1 month, 3 months, 6 months, and 12 months). A clinically significant reduction of pain and disability was observed after PRP injections. The VAS score decreased from 7/10 to 3/10, and the RMDQ score decreased from 13/24 to 5/24 after the last observation at 12 months. Improvement in quality of life was also observed at 12 months post-injection, as assessed by the SF-12 (Physical component score (PCS) from 43.3 to 68.3 and mental component score (MCS) from 40 to 60). A decrease in high signal intensity on T2WI was seen in the follow-up MRI compared to before the PRP injection. No adverse events following intradiscal PRP injection were observed during this period. In conclusion, intradiscal PRP injection is effective for LBP patients with type 1 Modic change. More prospective studies are needed to establish the safety and efficacy of PRP in type I modic change associated with low back pain.
Keywords
Low back pain, Modic change, Platelet rich plasma, Disability, Visual analogue scale, Roland‐Morris Disability Questionnaire, 12-item short form health survey.
Introduction
LBP is one of the most common causes of pain among the general population, and as many as 84% of people have experienced back pain at least once in a lifetime.[1,2] Most cases of lower back pain are self-limited; however, nearly 20% of patients experience lower back pain within six months of the initial development.[3] LBP is considered the leading cause of disability.[4,5] Global burden of disease (GBD) showed that the incidence rate of restricted LBP activity was estimated to be approximately 7.3%.[6]
Although several spine structures have been known as generators of pain, intervertebral disc (IVD) pathologies are responsible for nearly 40% of chronic low back pain cases.[7] During the process of degeneration, the cartilage dehydrates, and the disc height decreases, several proinflammatory mediators are produced, which are believed to cause persistent inflammation of the discs’ nucleus, granulation tissue may form, and abnormal nerve fibers can grow.[8,9,10] Modic changes (MC) are vertebral subchondral bone marrow changes that are visible in MRI and strongly associated with degenerative disc disease.[9,11,12] Type 1 MC is associated with LBP in both population-based and clinical samples.[13] Three main types of MC have been described. Type I shows decreased signal intensity on T1-weighted images (T1W) and increased signal intensity on T2-weighted images (T2W) and is thought to represent acute inflammatory changes in degenerative disc disease.[12] Type II MC shows increased signal intensity on both T1W and T2W; yellow marrow replacement in histopathological specimens. On the other hand, Type III MC shows decreased signal intensity on both T1W and T2W and is associated with extensive subchondral bone sclerosis. It has been suggested that type I may predict a fast-progressing and deforming type of disc degeneration.[9,12]
There is no gold standard treatment for modic change associated with low back pain. Recently, the use of autologous cells to treat degenerative disc diseases has become popular, including PRP, adipose mesenchymal stem cells, and bone marrow mesenchymal stem cells.[14] PRP has been widely studied to treat various musculoskeletal disorders; PRP contains higher concentrations of growth factors and is believed to promote healing and tissue formation.[15] However, there is a paucity of clinical evidence for the role of PRP therapy in Modic I change. Thus, we report a case to highlight the effect of PRP in type I Modic change associated with low back pain.
Case Presentation
A 65-year-old hypertensive, obese, female with osteopenia had visited the pain clinic, at Shaheed Suhrawardy Medical College and Hospital (ShSMCH), Dhaka with a history of persistent low back pain without any history of trauma or falls. She gave a history of taking betel leaves and nuts for about 25 years but denied any history of alcohol or tobacco use. Some of her maternal and paternal relatives had low back pain but she could not mention the cause of their LBP. Our patient has been suffering from LBP for about 18 months. She had been taking different analgesics for her low back pain but the pain did not resolve satisfactorily. She described her pain as achy and annoying, not allowing her to sit or stand for long periods. Physical examination findings revealed obesity with no significant scoliosis in a standing neutral position. Active lumbar range of motion (ROM) was slightly restricted due to pain. Straight leg raise (SLR) and Kemp tests were negative, excluding radiculopathy and facet joint arthropathy. Neurological examinations of the lower limbs and findings regarding the hips and pelvis were unremarkable. Examination of the back muscles revealed a slight increase in tone. MRI examination of the lumbar spine showed disc degeneration and herniation at multiple levels and modic changes (type I Modic) at the L4/5 disc. Her bone mineral density (BMD) test revealed a T score of -2 which was within the osteopenia range (-1 to -2.5). Her pain intensity was assessed by the VAS.[16] and her score was 7 out of 10. Pain-related disability was measured by the RMDQ.[17] which was 13 out of 24. Quality of life was assessed by the 12-item Short Form Health Survey (SF-12).[18] The physical composite score (PCS) and mental composite score (MCS) were 43.3 and 40 respectively. With proper counseling of the patient, we planned an intradiscal PRP injection for the treatment of LBP. Baseline characteristics are presented in Table 1.
| Characteristics | Value |
| Age (years) | 65 |
| Height (m) | 1.32 |
| Weight (kg) | 69 |
| BMI (kg/m2) | 39.6 |
| BMD (T score) | -2 |
| VAS score | 7 |
| RMDQ score | 13 |
| SF-12
PCS MCS |
43.3 40 |
| Duration of pain (months) | 18 |
Table 1: Baseline characteristics of the patient
Case Management
After obtaining informed consent, the patient was taken to the operating theatre. Antibiotics were administered by peripheral venous access to prevent infection before intradiscal PRP injection. PRP was made by the department of transfusion medicine, ShSMCH, and the platelet count was more than 1000000/ml. The patient was placed in a prone position on the X-ray operating table, and the L4-5 level was identified by counting vertebrae from X-ray images. With all aseptic precautions, the skin was infiltrated with 1% lignocaine. Then, a spinal needle (22-gauge, 150mm) was inserted into the nucleus pulposus (NP) of the L4/5 disc in the anteroposterior (AP) and lateral views under intermittent fluoroscopy. Approximately 2 mL of PRP was slowly injected through a syringe into the disc. After the procedure, the patient was observed in the post-operative ward for about an hour and found uneventful. The patient was advised to do activities of daily living and physical activity, such as exercise, at 7 days and 1 month postinjection, respectively. She was also advised not to take steroids and non-steroidal anti-inflammatory drugs (NSAIDs) for about 1 month, except in the case of particularly severe pain (VAS scores of 8 points or more). Follow-up surveys, including VAS, RMDQ, and any side effects, were carried out by phone at 1 week, 1 month, 3 months, 6 months, and 12 months following intradiscal PRP injections. Quality of life by SF-12 was measured after 1 month, 6 months, and 12 months. Subsequently, a follow-up MRI of the lumbar spine was done after 6 months of injection. Figure 1 shows the Modic change before and after PRP injection. A decrease in high signal intensity on T2WI was seen after PRP injection in the intervertebral disc at the L4/5 disc.

a

b

c

d
Figure 1: MRI shows modic change before (a,b) and after (c,d) PRP injection
Figure 2 shows the VAS score and RMDQ score after PRP injections at different points in time (lower scores indicate better). VAS score was reduced from 7 to 3 after 3 months, and no further reduction was observed at the last observation after 12 months. RMDQ score also decreased from 13 to 5 after 6 months and remained the same at 12 months.
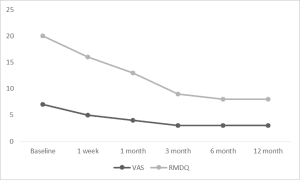
Figure 2: VAS score and RMDQ score at different time intervals
The quality of life was improved gradually, and the last observation at 12 months showed a PCS score of 68.3 and an MCS score of 60 (higher scores indicate better). Figure 3 shows the PCS and MCS scores at different points in time. No adverse effects like infection and nerve damage following the intradiscal PRP injections were observed.
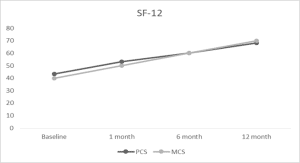
Figure 3: SF-12 score (PCS and MCS) at different time intervals
Discussion
Intervertebral discs (IVDs) and vertebral subchondral bone (VSB) are important anatomical elements of the spinal column affected by pain and degenerative pathology. Indeed, the whole can be considered as an intervertebral joint functional unit, composed of an IVD, the upper and lower vertebrae, and the facet joints.[19] In adults, an endplate bilayer of cartilage and bone (VSB) is located at the ends of each IVD, separating the vertebral bone from the IVD itself and preventing the central, gel-like, hydrated nucleus pulposus from bulging outward into the neighboring spinal canal and nerves. It is known that the VSB plays an important role in spinal function, maintaining IVD integrity and disc nutritional supply. Changes in IVD and VSB biomechanical and biochemical properties are associated with the development of back pain and degenerative disc disease (DDD). Some structural VSB alterations have been linked to disc degeneration.[20]
The prevalence of diagnosed spinal degenerative disease increases with age, is more common in females than in males, and is greater with obesity.[21] With osteopenia, bones are more likely to become sore from a lack of support, which can lead to back pain. On the other hand, chronic low back pain increases disability and has an increased incidence of osteopenia and osteoporosis.[22] Our patient belongs to an older age group, female, and obese, which may influence the risk of MC with low back pain. In a prospective cohort study.[23], The authors concluded that Modic type I was the only degenerative finding that predicted persistent symptoms. Mitra et al.[24] found a trend of higher pain intensity and disability scores among patients with Modic type I component and lower scores in patients with conversion of Modic type I to II. Treatment of Modic type I is still controversial, with some reports showing that antimicrobial agents are effective, whereas others reported that they were ineffective.[25]
In recent years, PRP therapy has been one of the regenerative medicines that has been attracting attention. A variety of growth factors, coagulation factors, adhesion molecules, cytokines, chemokines, and integrins are stored in platelets.[3,5] The growth factors released by platelets include transforming growth factor (TGF) β-1, vascular endothelial growth factor (VEGF), platelet-derived growth factor (PDGF), and epidermal growth factor (EGF); therefore, PRP injection in an IVD may result in cellular and tissue proliferation.[1,3,5,25]
This case study showed the effect of a single intradiscal autologous PRP injection in a patient with Modic change. The findings demonstrated clinically significant improvements in pain, physical function, and quality of life at several time points compared to baseline. Kawabata et al.[25] successfully demonstrated the efficacy of intradiscal administration of PRP in patients with Modic type I. They followed up with 10 patients after intradiscal PRP for up to 24 weeks and found significant improvement in the VAS, Oswestry disability index (ODI), and RMDQ. A prospective clinical trial on intradiscal platelet-rich plasma injection for discogenic LBP was conducted by Jain D et al.[1] demonstrated improvement of the numeric rating scale (NRS) and ODI score after PRP therapy. Another study evaluating the effectiveness of autologous PRP on discogenic low back pain (DLBP) at 48 weeks postinjection revealed a significant reduction of pain score (NRS) and improvement of SF-36 score.[26] In our study, we followed up for 12 months and found a clinically significant reduction of VAS and RMDQ scores as well as an improvement in SF-12 scores.
The process of Modic change in our patient was somehow reversed by PRP injection. This autologous platelet-rich plasma mimics the physiological repair process by releasing autologous growth factors (GFs) and creating a transient biological matrix. It can be considered that PRP treatment could stimulate the endogenous repair machinery and induce the healing of damaged spinal components to ultimately restore disc and vertebral bone homeostasis and an improvement in the functional anatomy of the end plate.[20] It is difficult to determine whether Modic type 1 is the cause of LBP. Discography may be necessary to diagnose Modic change accurately as the cause of LBP. However, discography, an invasive test, was not performed in this study because a significant association was established between MC and LBP.[25]
Only a few reports demonstrate MRI improvements in disc degeneration and Modic change after PRP treatment. As MRI provides more detailed information, the case presented here shows appreciable MRI improvements in terms of decreasing high-signal intensity on T2WI after 6 months of PRP therapy.[20,25] Other modalities like intradiscal steroid injections, anti-tumor necrosis factor (TNF)-α antibodies, and antibiotic administration, have been reported to have short-term efficacy in Modic change, but long-term results are unknown. Albert et al. treated patients with Modic type I with antibiotics for 100 days and reported that the VAS of patients with LBP improved from 67 to 37 mm after 1 year.[27]
Conclusion
Intradiscal injection of PRP can relieve pain and improve lumbar function as well as quality of life in patients with LBP associated with Modic type I. It also promotes morphological changes of Modic type I, which is demonstrated with MRI analysis. Further randomized controlled clinical trials are needed to evaluate the safety and efficacy of this injection therapy for LBP with Modic type I.
References
- Jain D, Goyal T, Verma N, Paswan AK, Dubey RK. Intradiscal platelet-rich plasma injection for discogenic low back pain and correlation with platelet concentration: a prospective clinical trial. Pain Med. 2020;21(11):2719-2725. doi:10.1093/pm/pnaa254 PubMed | Crossref | Google Scholar
- Manchikanti L, Singh V, Falco FJ, Benyamin RM, Hirsch JA. Epidemiology of low back pain in adults. Neuromodulation. 2014;17 Suppl 2:3-10. doi:10.1111/ner.12018 PubMed | Crossref | Google Scholar
- Chang MC, Park D. The effect of intradiscal platelet-rich plasma injection for management of discogenic lower back pain: a meta-analysis. J Pain Res. 2021;14:505-512. doi:10.2147/JPR.S292335 PubMed | Crossref | Google Scholar
- Hartvigsen J, Hancock MJ, Kongsted A, et al. What low back pain is and why we need to pay attention. Lancet. 2018;391(10137):2356-2367. doi:10.1016/S0140-6736(18)30480-X PubMed | Crossref | Google Scholar
- Levi D, Horn S, Tyszko S, Levin J, Hecht-Leavitt C, Walko E. Intradiscal platelet-rich plasma injection for chronic discogenic low back pain: preliminary results from a prospective trial. Pain Med. 2016;17(6):1010-1022. doi:10.1093/pm/pnv053 PubMed | Crossref | Google Scholar
- GBD 2017 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1859-1922. doi:10.1016/S0140-6736(18)32335-3 PubMed | Crossref
- Schwarzer AC, Aprill CN, Derby R, Fortin J, Kine G, Bogduk N. The prevalence and clinical features of internal disc disruption in patients with chronic low back pain. Spine (Phila Pa 1976). 1995;20(17):1878-1883. doi:10.1097/00007632-199509000-00007 PubMed | Crossref | Google Scholar
- Peng B, Hou S, Wu W, Zhang C, Yang Y. The pathogenesis and clinical significance of a high-intensity zone (HIZ) of lumbar intervertebral disc on MR imaging in the patient with discogenic low back pain. Eur Spine J. 2006;15(5):583-587. doi:10.1007/s00586-005-0892-8 PubMed | Crossref | Google Scholar
- Jensen TS, Karppinen J, Sorensen JS, Niinimäki J, Leboeuf-Yde C. Vertebral endplate signal changes (Modic change): a systematic literature review of prevalence and association with non-specific low back pain. Eur Spine J. 2008;17(11):1407-1422. doi:10.1007/s00586-008-0770-2 PubMed | Crossref | Google Scholar
- Sehgal N, Fortin JD. Internal disc disruption and low back pain. Pain Physician. 2000;3(2):143-157. Internal disc disruption and low back pain
- Modic MT, Steinberg PM, Ross JS, Masaryk TJ, Carter JR. Degenerative disk disease: assessment of changes in vertebral body marrow with MR imaging. Radiology. 1988;166(1 Pt 1):193-199. doi:10.1148/radiology.166.1.3336678 PubMed | Crossref | Google Scholar
- Cao P, Jiang L, Zhuang C, et al. Intradiscal injection therapy for degenerative chronic discogenic low back pain with end plate Modic changes. Spine J. 2011;11(2):100-106. doi:10.1016/j.spinee.2010.07.001 PubMed | Crossref |
Google Scholar - Kjaer P, Korsholm L, Bendix T, Sorensen JS, Leboeuf-Yde C. Modic changes and their associations with clinical findings. Eur Spine J. 2006;15(9):1312-1319. doi:10.1007/s00586-006-0185-x PubMed | Crossref | Google Scholar
- Everts P, Onishi K, Jayaram P, Lana JF, Mautner K. Platelet-rich plasma: new performance understandings and therapeutic considerations in 2020. Int J Mol Sci. 2020;21(20):7794. doi:10.3390/ijms21207794
PubMed | Crossref | Google Scholar - Chang Y, Yang M, Ke S, Zhang Y, Xu G, Li Z. Effect of platelet-rich plasma on intervertebral disc degeneration in vivo and in vitro: a critical review. Oxid Med Cell Longev. 2020;2020:8893819. doi:10.1155/2020/8893819 PubMed | Crossref | Google Scholar
- Shafshak TS, Elnemr R. The visual analogue scale versus numerical rating scale in measuring pain severity and predicting disability in low back pain. J Clin Rheumatol. 2021;27(7):282-285. doi:10.1097/RHU.0000000000001320 PubMed | Crossref | Google Scholar
- Roland M, Fairbank J. The Roland-Morris Disability Questionnaire and the Oswestry Disability Questionnaire. Spine (Phila Pa 1976). 2000;25(24):3115-3124. doi:10.1097/00007632-200012150-00006 PubMed | Crossref | Google Scholar
- Luo X, George ML, Kakouras I, et al. Reliability, validity, and responsiveness of the short form 12-item survey (SF-12) in patients with back pain. Spine (Phila Pa 1976). 2003;28(15):1739-1745. doi:10.1097/01.BRS.0000083169.58671.96 PubMed | Crossref | Google Scholar
- Anitua E, Padilla S. Biologic therapies to enhance intervertebral disc repair. Regen Med. 2018;13(1):55-72. doi:10.2217/rme-2017-0111 PubMed | Crossref | Google Scholar
- Kirchner F, Pinar A, Milani I, Prado R, Padilla S, Anitua E. Vertebral intraosseous plasma rich in growth factor (PRGF-Endoret) infiltrations as a novel strategy for the treatment of degenerative lesions of endplate in lumbar pathology: description of technique and case presentation. J Orthop Surg Res. 2020;15(1):72. doi:10.1186/s13018-020-01605-w PubMed | Crossref | Google Scholar
- Parenteau CS, Lau EC, Campbell IC, Courtney A. Prevalence of spine degeneration diagnosis by type, age, gender, and obesity using Medicare data. Sci Rep. 2021;11(1):5389. doi:10.1038/s41598-021-84724-6 PubMed | Crossref | Google Scholar
- Gaber TA, McGlashan KA, Love S, Jenner JR, Crisp AJ. Bone density in chronic low back pain: a pilot study. Clin Rehabil. 2002;16(8):867-870. doi:10.1191/0269215502cr558oa PubMed | Crossref | Google Scholar
- Jensen OK, Nielsen CV, Sørensen JS, Stengaard-Pedersen K. Type 1 Modic changes was a significant risk factor for 1-year outcome in sick-listed low back pain patients: a nested cohort study using magnetic resonance imaging of the lumbar spine. Spine J. 2014;14(11):2568-2581. doi:10.1016/j.spinee.2014.02.018 PubMed | Crossref | Google Scholar
- Zhang YH, Zhao CQ, Jiang LS, Chen XD, Dai LY. Modic changes: a systematic review of the literature. Eur Spine J. 2008;17(10):1289-1299. doi:10.1007/s00586-008-0758-y PubMed | Crossref | Google Scholar
- Kawabata S, Hachiya K, Nagai S, et al. Autologous platelet-rich plasma administration on the intervertebral disc in low back pain patients with Modic type 1 change: report of two cases. Medicina (Kaunas). 2023;59(1):112. doi:10.3390/medicina59010112 PubMed | Crossref | Google Scholar
- Zhang J, Liu D, Gong Q, Chen J, Wan L. Intradiscal autologous platelet-rich plasma injection for discogenic low back pain: a clinical trial. Biomed Res Int.2022:9563693. doi:10.1155/2022/9563693 PubMed | Crossref | Google Scholar
- Albert HB, Sorensen JS, Christensen BS, Manniche C. Antibiotic treatment in patients with chronic low back pain and vertebral bone edema (Modic type 1 changes): a double-blind randomized clinical controlled trial of efficacy. Eur Spine J. 2013;22(4):697-707. doi:10.1007/s00586-013-2675-y PubMed | Crossref | Google Scholar
Acknowledgments
We would like to thank Dr. Md. Habibur Rahman, Assistant Professor, Department of Transfusion Medicine, Shaheed Suhrawardy Medical College and Hospital, Dhaka-1207.
Funding
Not reported
Author Information
Corresponding Author:
Md Mostafa Kamal
Department of Anaesthesia
Shaheed Suhrawardy Medical College and Hospital, Bangladesh
Email: dr.mostafakamal85@gmail.com
Co-Authors:
Shahara Afroz
Department of Anaesthesia and Pain Medicine
Evercare Hospital, Bangladesh
AKM Akhtaruzzaman
Department of Anaesthesia, Analgesia and Intensive Care Medicine
Bangabandhu Sheikh Mujib Medical University, Bangladesh
Authors Contributions
All authors contributed to the conceptualization, investigation, and data curation by acquiring and critically reviewing the selected articles. They were collectively involved in the writing – original draft preparation, and writing – review & editing to refine the manuscript. Additionally, all authors participated in the supervision of the work, ensuring accuracy and completeness. The final manuscript was approved by all named authors for submission to the journal.
Informed Consent
Not applicable
Conflict of Interest Statement
Not applicable
Guarantor
Not applicable
DOI
Cite this Article
Md MK, Shahara A, AKM A. Intradiscal Platelet-Rich Plasma Injection for Type I Modic Change Associated with Low Back Pain in Osteopenia. medtigo J Med. 2024;2(4):e30622425. doi:10.63096/medtigo30622425 Crossref









