Author Affiliations
Abstract
Background: Deep vein thrombosis (DVT) is a major postoperative complication with potentially catastrophic sequela of life-threatening pulmonary embolism. Major surgeries, especially those that require a long period of immobility and tissue damage, pose a high risk of DVT. It is also important to determine how it occurs in various surgical units so that countermeasures can be implemented.
Aim: This study aimed to determine the incidence of DVT following major surgeries in the General Surgery and Gynecological Surgery departments at Saidu Group of Teaching Hospitals (SGTH), Swat.
Methodology: A descriptive observational study was carried out on 270 adult patients undergoing major elective or emergency surgery. A structured checklist and clinical assessment were used to collect data. Suspected DVT cases were confirmed via Doppler ultrasound. We used a statistical package for the social sciences (SPSS), version 27, to analyze data and applied descriptive statistics and chi-square tests.
Results: The overall incidence of DVT was 10.4%. The occurrence of DVT was higher with General (12.5%) and lower with Gynecological (7.3%) Surgery. There was a significant correlation between the type of surgery and the incidence of DVT (p = 0.033).
Conclusion: Among major surgeries, DVT is a significant postoperative complication, particularly in general surgery patients. It can be reduced by strengthening thromboprophylaxis practices and maximizing early mobilization.
Keywords
Deep vein thrombosis, Incidence, Major surgery, General surgery, Gynecological surgery, Postoperative complications.
Introduction
Deep vein thrombosis (DVT) is the presence of a blood clot (thrombus) in one of the deep veins, most frequently in the legs.[1] Major surgery is a high-invasive, large-scope surgery that frequently necessitates general anesthesia; this most commonly takes the form of orthopedic, abdominal, cardiac, or oncologic surgery. Incidence of DVT is used to refer to the frequency at which new cases of DVT occur in a given time and among a given population.[2] A severe postoperative complication is the postoperative DVT, because surgery causes immobility, endothelial injury, and hypercoagulable states.[3] DVT can cause pulmonary embolism (PE) that can be deadly when undetected or untreated. The occurrence of DVT in different types of major procedures is important in the recognition of the condition and early intervention.[4]
Globally, DVT affects a significant proportion of surgical patients. According to the World Health Organization and other national health agencies, postoperative DVT has been observed to be one of the main preventable causes of hospital-related deaths.[5] Research and experiments have established that the prevalence of DVT varies between 15 and 60 % according to the surgical procedure, risks of the host, and the application of thromboprophylaxis.[6] Orthopedic rates, e.g., of hip or knee replacement, are very high, possibly exceeding 40 % in the absence of prophylaxis. Conversely, clinically meaningful and yet lower rates of DVT are encountered in general surgeries, including abdominal or pelvic procedures. Very little data exists in South Asia, with the burden estimated to be under-reported, likely because of low levels of screening and awareness.[7]
A significant clinical issue is that DVT can manifest itself with no apparent symptoms and progress into serious, life-threatening complications. Typical manifestations of pain, oedema, erythema, and warmth in the ipsilateral limb can be minor or inconspicuous, and diagnosis depends on Doppler ultrasound or D-dimer assays.[6] Time immobility, particularly twilight and following significant surgery, is a considerable predisposing factor in the development of thrombus. Therefore, finding surgeries that possess the most risk indicators is the key to specific prevention tactics, like pharmacologic anticoagulants or compression devices.[8]
Postoperative DVT depends on various risk factors such as age greater than 60, obesity, malignancy, personal history of thromboembolic disease, hormone treatment, and hereditary thrombosis. The nature and length of surgery are also factors. Orthopedic procedures, especially those performed on the pelvis or lower extremities, have a higher tendency to create DVT because of direct vascular injury and compromised venous return. Oncologic surgeries carry an increased risk due to cancer-associated hypercoagulability.[9] Surgery of the heart and nervous system is also at high risk because of the prolonged period of surgery and limited post-surgery mobility.[10]
The prevention of DVT among surgical patients has become a norm of care across most advanced healthcare systems. Risk stratification and sensible application of thromboprophylaxis preoperatively and during the postoperative phases are suggested in clinical guidelines.[11] Even though such progress is made, there is a lack of compliance with the guidelines, especially in low-resource environments, which results in avoidable complications. An evaluation of the occurrence of DVT in various types of surgeries will not only provide an understanding of the plausibility of the present protocol but will also emphasize the necessity of optimization of perioperative care and education of medical practitioners.[12]
The prior research has been mostly on specific surgical specialties, including orthopedics or oncology, and in high-income settings with access to standardized thromboprophylaxis. Nevertheless, limited information exists regarding overall data to contrast the incidence of DVT between some major surgical procedures of various healthcare institutions and in resource-limited areas specifically.[13] Such a gap complicates the efficient distribution of available resources or the adaptation of thromboprophylaxis protocols to groups of increased risk. The requirement of local, procedure-specific information is understood, particularly to inform national health policies and enhance clinical outcomes.[14]
It is this gap that this study focuses on filling by ascertaining the frequency of DVT among patients who receive various kinds of major surgeries. This study will add to procedural-based risk by comparing and contrasting the prevalence of orthopedic, lower abdominal, cardiac, and oncological surgery. Clinicians can use the findings in risk assessment and management strategies, ensuring risk management and maximizing the postoperative outcomes and patient safety by implementing more accurate interventions based on evidence.
Methodology
The descriptive observational study design was used to establish DVT incidence after various categories of major surgery. It is done under the SGTH based in Swat in the departments of General Surgery and Gynecological Surgical Services. The adult patients aged 18 years and above who had undergone big surgical procedures in the identified wards formed the target population. A total of 900 surgical patients were estimated to be the population, using the OpenEpi sample size calculator, 95% level of certainty, and a margin of error of 5%. The final sample size was determined to be 270. Patients were selected through non-probability consecutive sampling.
Inclusion criteria entailed patients who were having major elective or emergency surgical procedures under general or spinal anesthesia and had postoperative stays of three days or more. The study excluded patients who had a known history of DVT, clotting disorders, or were already using anticoagulants.
Data collection: A structured checklist was conducted to collect data, containing demographic data, the type and duration of surgery, comorbidities, postoperative mobility status, and whether thromboprophylaxis was used. Postoperative observation of patients was done to detect clinical manifestations of DVT, including unilateral leg swelling, pain, tenderness, and redness. Every suspected DVT case was confirmed by Doppler ultrasound, which was carried out by radiologists at SGTH.
Data analysis: Data were analyzed using SPSS version 27. The patient characteristics and DVT incidence were summarized using descriptive statistics, frequencies, percentages, and means. The chi-square test was used in an attempt to evaluate the association between the type of surgery and DVT occurrence, with a significance level of p < 0.05.
Results
Demographic characteristics: Most participants were female (58.5%), with males comprising 41.5% of the sample. Most patients belonged to the 31–50 years age group (40%), followed by 51+ years (33.3%). A higher proportion of surgeries were performed in the general surgery department (70.3%) compared to gynae surgery (29.7%).
| Variable | Category | Frequency (n) | Percentage (%) |
| Gender | Male | 112 | 41.5% |
| Female | 158 | 58.5% | |
| Age group | 18–30 years | 72 | 26.7% |
| 31–50 years | 108 | 40.0% | |
| 51+ years | 90 | 33.3% | |
| Department | General surgery | 190 | 70.3% |
| Gynae surgery | 80 | 29.7% |
Table 1: Demographic characteristics of surgical patients (N = 270)
Clinical and surgical characteristics: Most surgeries were elective (68.5%), and over half of the procedures lasted less than 2 hours (53.3%). On the first postoperative day, 64.4% of patients were mobile. Thromboprophylaxis was administered to 73.3% of the patients, while 26.7% did not receive it (Table 2).
| Variable | Category | Frequency (n) | Percentage (%) |
| Type of surgery | Elective | 185 | 68.5% |
| Emergency | 85 | 31.5% | |
| Duration of surgery | <2 hours | 144 | 53.3% |
| ≥2 hours | 126 | 46.7% | |
| Postoperative mobility (Day 1) | Mobile | 174 | 64.4% |
| Immobile | 96 | 35.6% | |
| Thromboprophylaxis given | Yes | 198 | 73.3% |
| No | 72 | 26.7% |
Table 2: Clinical and surgical characteristics
DVT was diagnosed with 10.4% of the patients. The remaining 89.6% showed no signs of DVT among the total sample of 270 surgical patients (Figure 1).
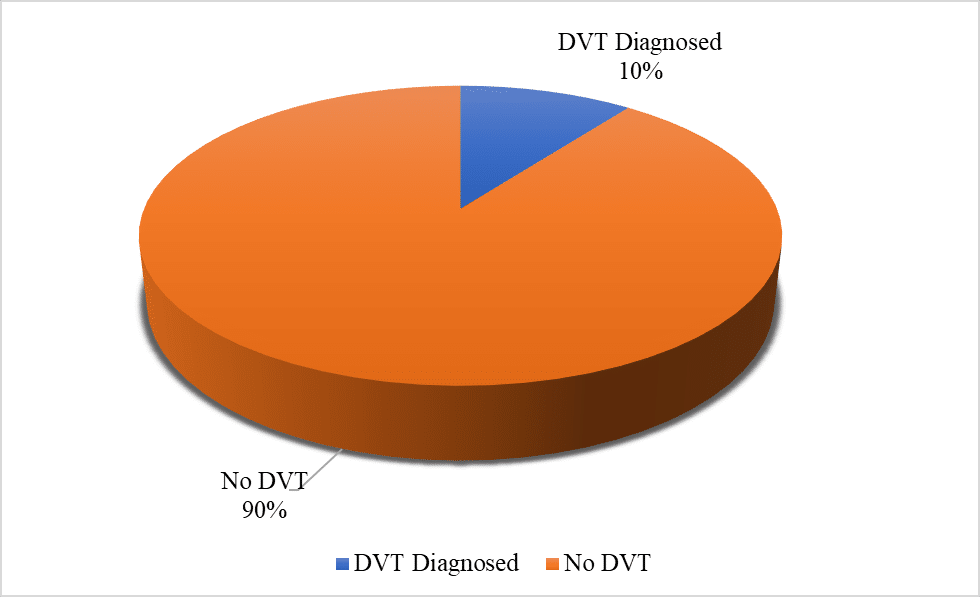
Figure 1: Incidence of DVT (N = 270)
DVT was more common among patients in the General Surgery department, with an incidence of 12.5%. In comparison, the Gynecological Surgery department had a lower DVT incidence of 7.3% (Table 3).
| Department | Total patients | DVT cases (n) | Percentage (%) |
| General surgery | 190 | 24 | 12.5% |
| Gynecological surgery | 80 | 6 | 7.3% |
Table 3: DVT cases by type of surgery (N = 270)
The chi-square test showed a statistically significant association between the type of surgery and DVT occurrence (χ² = 4.521, p = 0.033), indicating that surgery type influences the risk of developing DVT (Table 4).
| Variable | Chi-square (χ²) | p-value | Significance |
| Type of surgery vs. DVT | 4.521 | 0.033 | Significant (p < 0.05) |
Table 4: Association between surgery type and DVT occurrence (Chi-square test)
Discussions
In the current study, the incidence of DVT after various major surgical procedures carried out at SGTH, Swat, was ascertained. A total of 270 surgical patients were included in the study, of which 28 (10.4%) had DVT after the surgery. Most of these cases were in the department of General Surgery (12.5%) as opposed to the department of gynecological surgery (7.3%). Results indicate that the risk of developing postoperative DVT significantly depends on the type of surgery performed, which is supported by the chi-square test (p = 0.033) showing a statistically significant correlation.[15]
The figures are also in line with previous literature that reveals increased risk of DVT in the general population and orthopedic surgical cases, which occur due to increased tissue trauma, longer operative time, and increased immobility.[16] According to the study, surgical patients, especially those involving the abdomen and pelvis, have a high risk of thromboembolic complications in the absence of proper thromboprophylaxis. The present research helps to corroborate this fact as 73.3 percent of patients were administered thromboprophylaxis, yet DVT occurred in a significant percentage of the cases, indicating that the risk of DVT has multifactorial origins.[17]
Conversely, the reduced incidence of DVTs in surgical patients undergoing gynecological surgery reported in this study concurs with those who reported fewer thrombotic complications in short and less invasive surgery, particularly patients who undergo early postoperative movements.[18] Nevertheless, even gynecological operations pose a 7.3 percent risk of DVT, which should warn about careful consideration of even such patients without excluding them from any risk-prevention measures.
Interestingly, the incidence rate change overall is slightly less than that of well-defined high-risk surgical groups across the planet, where it may increase to more than 20 percent, in the absence of appropriate prophylaxis.[19] It may be explained by the improved perioperative care, mobility practices, and the use of anticoagulants routinely in the study. It can, however, also indicate underdiagnosis caused by the low application of routine Doppler screening in asymptomatic patients.
The connection between postoperative immobilization and the risk of DVT was identified as well, with only 35.6 per cent of patients being immobile on the first day of surgery. This is in line with the results of who highlighted the importance of early ambulation as a key factor in the prevention of thrombotic episodes.[20] The large percentage of immobile patients in this study is a sign of the need for increased nursing protocols involving early mobilization of patients, especially among those in general surgery.[21]
Another finding of the study showed that prolonged surgical events (2+hours) were related to DVT incidences; an observation consistent with the current body of literature.[22] Longer duration of operation is associated with higher chances of developing venous stasis and endothelial injury, two factors that make up the Virchow triad and lead to thrombus development. Therefore, preoperative risk factors should include surgical duration as a risk consideration.[23]
As a conclusion, the results of this study suggest that the type of surgery is strongly associated with the occurrence of DVT. Patients of general surgery were more vulnerable than gynecological surgery patients. Despite the popularity of thromboprophylaxis, the rates of DVT were observed at 10.3% which indicates that more stringent assessment, protection, and early diagnosis practices are necessary. Future studies ought to support multicentric model and standard screening procedures to detect possible silent DVT and report a real incidence figure of the condition.
Recommendations
Implement routine DVT risk assessment: Standardized preoperative assessment of the risk of DVT based on validated scales is important to find high-risk surgical patients and implement specific preventive strategies.
Enhance postoperative mobilization protocols: Ambulation should be encouraged early, in the first 24 hours whenever possible after the surgery, to minimize the risk of thrombus formation and venous stasis.
Ensure consistent use of thromboprophylaxis: Pharmacological and mechanical thromboprophylaxis should be highly adherent to clinical guidelines according to individual patient risk factors and surgery type.
Provide staff training and awareness programs: Surgical and nursing teams should receive regular training on DVT prevention, early signs, and intervention in time.
Integrate routine doppler screening for high-risk cases: Doppler ultrasound screening can be considered in high-risk patients and those with symptoms after surgery to start treatment and manage DVT early.
Develop department-specific DVT protocols: Departments like General Surgery and Gynecology deserve independent protocols, given that the incidence of DVT and surgical practice is different.
Promote patient education: Instruct surgical patients regarding DVT risk, signs and symptoms, and the need to mobilize and comply with required prophylactic measures during hospital stay and outpatient visits.
Conclusion
In this study, the conclusion was that DVT is a major post-operative complication in patients who have undergone major surgeries, especially in general surgery rather than gynecological surgery. The total incidence was 10.4 percent, with the type of surgery and the DVT occurrence having a significant correlation (p = 0.033). Even though most patients were on thromboprophylaxis, there was still a significant occurrence of DVT, therefore also underscoring the multifactorial risk factors of DVT, with immobility and lengthy surgical stays among them. These data indicate the necessity of preoperative risk assessment capture, the regular use of evidence-based prophylaxis, and early rehabilitation after surgery as measures to minimize DVT. Routine monitoring and personalized prevention measures need to be part of surgical care pathways to improve patient safety and outcomes.
References
- Duffett L. Deep Venous Thrombosis. Ann Intern Med. 2022;175(9):ITC129-ITC144. doi:10.7326/AITC202209200
PubMed | Crossref | Google Scholar - International Society for Stem Cell Research. 23rd human proteome organization world congress. 2024.
23rd human proteome organization world congress - Noumegni SR, Hoffmann C, Tromeur C, et al. Frequency and incidence of arterial events in patients with venous thromboembolism compared to the general population: A systematic review and meta-analysis of cohort studies. Thromb Res. 2021;203:172-185. doi:10.1016/j.thromres.2021.05.009
PubMed | Crossref | Google Scholar - Castellana G, Intiglietta P, Dragonieri S, et al. Incidence of deep venous thrombosis in patients with both Pulmonary Embolism and COPD. Acta Biomed. 2021;92(3):e2021210. doi:10.23750/abm.v92i3.11258
PubMed | Crossref | Google Scholar - Mohamed Ahmed M, AboZead S, Yousef A, Taha S. Effect of implementing nursing educational protocol on reducing deep venous thrombosis among orthopedic surgery patients. Minia Scientific Nursing Journal. 2021;009(1):111-117. doi:10.21608/msnj.2021.190448
Crossref | Google Scholar - Osman M, Abd El-Hay S, Ewees W, Bahgat Z. Effect of educational program for nurses’ performance and clinical outcome regarding occurrence of deep vein thrombosis among major orthopedic surgery patients. Tanta Sci Nurs J. 2024;33(2):108-128. doi:10.21608/tsnj.2024.350970
Crossref | Google Scholar - Ma J, Du P, Qin J, et al. Incidence and risk factors predicting deep venous thrombosis of lower extremity following spinal fractures. Sci Rep. 2021;11(1):2441. doi:10.1038/s41598-021-82147-x
PubMed | Crossref | Google Scholar - Alanezi RD, Alenazi AMJ, Alenzi SAL, et al. Nursing strategies to avoid DVT among postoperative patients: Comprehensive review. J Int Crisis Risk Commun Res. 2024;7(S11):1502-1517. doi:10.63278/jicrcr.vi.1419
Crossref | Google Scholar - Ortega MA, Fraile-Martínez O, García-Montero C, et al. Understanding Chronic Venous Disease: A Critical Overview of Its Pathophysiology and Medical Management. J Clin Med. 2021;10(15):3239. doi:10.3390/jcm10153239
PubMed | Crossref | Google Scholar - Fuenmayor MAG, Bustamante GVS, Zurita EPA, et al. Risk factors for deep venous thrombosis in patients undergoing orthopedic surgical procedures. doi:10.5281/ZENODO.6983656
Crossref | Google Scholar - Yu X, Wu Y, Ning R. The deep vein thrombosis of lower limb after total hip arthroplasty: what should we care. BMC Musculoskelet Disord. 2021;22(1):547. doi:10.1186/s12891-021-04417-z
PubMed | Crossref | Google Scholar - Basli AA, Kurt D. Deep vein thrombosis risk and preventive nursing practices in surgical patients: A descriptive cross-sectional study. J Vasc Nurs. 2025;43(1):27-32. doi:10.1016/j.jvn.2024.12.001
PubMed | Crossref | Google Scholar - Luo L, Kou R, Feng Y, Xiang J, Zhu W. Cost-Effective Machine Learning Based Clinical Pre-Test Probability Strategy for DVT Diagnosis in Neurological Intensive Care Unit. Clin Appl Thromb Hemost. 2021;27:10760296211008650. doi:10.1177/10760296211008650
PubMed | Crossref | Google Scholar - Zamora T, Botello E, Jenkins T, et al. Global and regional disparities in access to specialist sarcoma services. Bone Jt Open. 2025;6(4):425-431. doi:10.1302/2633-1462.64.BJO-2024-0208.R1
PubMed | Crossref | Google Scholar - Leversedge C, Castro S, Appiani LMC, Kamal R, Shapiro L. Patient Follow-up After Orthopaedic Outreach Trips – Do We Know Whether Patients are Improving?. World J Surg. 2022;46(10):2299-2309. doi:10.1007/s00268-022-06630-w
PubMed | Crossref | Google Scholar - Theochari CA, Theochari NA, Mylonas KS, et al. Venous Thromboembolism Following Major Abdominal Surgery for Cancer: A Guide for the Surgical Intern. Curr Pharm Des. 2022;28(10):787-797. doi:10.2174/1381612828666220217140639
PubMed | Crossref | Google Scholar - Dancz CE, Tavakoli A, Shabalova A. Diagnosis and management of delayed postoperative complications in gynecology: Neuropathy, wound complications, fistulae, thromboembolism, pelvic organ prolapse, and cuff complications. In: Handbook of Gynecology. Springer International Publishing; 2023:893-910.
Diagnosis and Management of Delayed Postoperative Complications in Gynecology: Neuropathy, Wound Complications, Fistulae, Thromboembolism, Pelvic Organ Prolapse, and Cuff Complications - Erika Weisbord. Peri- and post-operative optimization in advanced gynecological oncology. Lietuvos sveikatos mokslų universitetas. 2022.
Peri- and Post-Operative Optimization in Advanced Gynecological Oncology - Moloughi S, Pourhoseini SA, Jafari M, Dalili A. Unilateral diaphragmatic paralysis, A rare complication of laparoscopic resection of an ovary cyst: A case report. J Obstet Gynecol Cancer Res. 2025;10(6):499-502. doi:10.30699/jogcr.10.6.499
Crossref | Google Scholar - Bernate JD, López AM, Rojas Liévano J, et al. Preoperative anticoagulation and its impact on surgical timing and postoperative outcomes in hip fracture surgery: a retrospective study at an Orthogeriatrics Clinical Care Center in Colombia. Eur J Orthop Surg Traumatol. 2025;35(1):170. doi:10.1007/s00590-025-04286-5
PubMed | Crossref | Google Scholar - Andronic D, Andronic O, Ammann E, Pravin E, Cubberley R. Outcomes of different perioperative management strategies of patients on chronic anticoagulation in elective total hip and knee arthroplasty: a systematic review. Fam Pract. 2024;41(5):629-637. doi:10.1093/fampra/cmae020
PubMed | Crossref | Google Scholar - Hillegass E, Lukaszewicz K, Puthoff M. Role of Physical Therapists in the Management of Individuals at Risk for or Diagnosed With Venous Thromboembolism: Evidence-Based Clinical Practice Guideline 2022. Phys Ther. 2022;102(8):pzac057. doi:10.1093/ptj/pzac057
PubMed | Crossref | Google Scholar - De Maeseneer MG, Kakkos SK, Aherne T, et al. Editor’s Choice – European Society for Vascular Surgery (ESVS) 2022 Clinical Practice Guidelines on the Management of Chronic Venous Disease of the Lower Limbs. Eur J Vasc Endovasc Surg. 2022;63(2):184-267. doi:10.1016/j.ejvs.2021.12.024
PubMed | Crossref | Google Scholar
Acknowledgments
The authors would like to express their sincere gratitude to Dr. Shah Hussain, Principal/Assistant Professor, Zalan College of Nursing, Swat, for his invaluable supervision, guidance, and support throughout the course of this study.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author Information
Corresponding Author:
Sami Ur Rahman
Department of Surgery
SGTH, Swat, Pakistan
Email: sk285881@gmail.com
Co-Authors:
Atiqa Naz Bibi
Department of Gynae and OBS
SGTH, Swat, Pakistan
Munib Ahmad Khan
Department of Surgery
SGTH, Swat, Pakistan
Javairia Riaz Masood
Department of Surgery
SGTH, Swat, Pakistan
Syed Wasim Ahmad
Department of Surgery
SGTH, Swat, Pakistan
Nazli Akbar
Department of Gynae and OBS
SGTH, Swat, Pakistan
Shah Hussain
Department of Nursing
Zalan College of Nursing, Swat, Pakistan
Authors Contributions
Dr. Sami Ur Rahman was responsible for data collection and data analysis. Dr. Atiqa Naz Bibi and Dr. Javairia Riaz Masood contributed to data collection and conducted the literature review. Dr. Munib Ahmad Khan, Dr. Syed Wasim Ahmad, and Dr. Nazli Akbar were involved in data collection and data organization. Dr. Shah Hussain handled data analysis and interpretation.
Ethical Approval
Ethical approval was obtained from SGTH, Swat (Ref. No. SGTH/IRB/2025/56).
Conflict of Interest Statement
The authors declare no conflict of interest.
Guarantor
Dr. Sami Ur Rahman is the guarantor of this study and takes full responsibility for the integrity of the data and the accuracy of the data analysis.
DOI
Cite this Article
Rahman SU, Bibi AN, Khan MA, et al. Incidence of deep vein thrombosis following different types of major surgeries. medtigo J Anesth Pain Med. 2025;1(2):e3067121. doi:10.63096/medtigo3067121 Crossref






