Author Affiliations
Abstract
A critical issue in healthcare today is the insufficient skill level among professionals in guiding patients to effectively address and manage their physical health challenges. The capstone project involved the development of an introductory motivational interviewing training curriculum. The analysis, design, development, implementation, and evaluation (ADDIE) model was used to determine the need for this product, design the content and processes, and develop the finished curriculum. This curriculum’s components consist of a motivational interviewing (MI) facilitator’s guide and a corresponding participant’s guide. It follows crucial skills associated with MI’s style and its focus on the MI skills of engaging, focusing, evoking, and planning. Once implemented, this project intends to enhance health care management practice by engaging patients in health care services to support and produce positive health outcomes. The MI training curriculum consists of two components: an instructor’s guide and a participant guide. The curriculum is a tool that provides the necessary resources to teach the interpersonal aspects of communication, the style and delivery of care professionals to their patients, and how it impacts patients’ decisions. The developed curriculum product improves health management staff members’ skill sets and encourages positive health outcomes through MI training. This enhancement in practice will impact the organization by increasing patient engagement in health coaching and disease management.
Keywords
Motivational interviewing, Capstone project, Healthcare professionals, Patient engagement, Health outcomes.
Introduction
Member engagement and participation within the healthcare system are crucial aims and goals, and without them, the organization could fail to deliver the required services. The capstone report delves into the importance of motivational interviewing (MI) for the capstone site, an organization within the health insurance industry. The organization selected in the current report is a team of uniquely organized medical businesses that provide healthcare services to different populations. More importantly, the project focuses on the care team that deals with the healthcare management of patients with the intent to change patients’ behavior for improved health. The professionalism with which the patients are engaged is crucial because patient-centered care is the organization’s mission and vision. MI has proven to be an adequate means to empower patients to make personal behavioral change decisions to improve their medical condition. The capstone project delivers a set of MI training materials, a facilitator’s guide, and a participant guide. Using the ADDIE model, this curriculum was designed to improve healthcare professionals’ skill sets and support the efficiency and effectiveness of available learning solutions.[1] The deliverable is justified by a range of research indicating MI’s benefits for both individuals and organizations. The skillsets of practitioners who deliver MI continue to be ineffective.[2] For these reasons, the project assumes importance in the care management sector, and the instructional designer is qualified to present this change based on educational and professional background.
The capstone project aligns with the educational leadership and management specialization. Two criteria were chosen to rationalize this project’s topic based on Capella’s programs of professional practice. The first involves changes and innovation, and the other is research, literature, and relevant information for evidence-based decision-making. The curriculum project promotes changes within healthcare professionals’ skill sets, which were studied prior to and observed to improve professional communication and patient engagement. Technology in the healthcare industry can be utilized to increase patients’ understanding and ease healthcare delivery. This innovation applies to online platforms used to deliver training sessions, especially during the current pandemic. The project supports the instructional designer’s professional practice and improves the practice of other individuals participating in MI training. Additionally, learning is a continuous process and a requirement for any healthcare professional. This project ensures that the most recent literature and science are reflected and applied to delivering healthcare services.
The problem addressed in this curriculum project is the gap in the health professionals’ skill level in helping patients address and manage their physical health conditions.[3] The problem indicates the need for organizations to create learning systems that provide the necessary training to help patients make the right decisions through an effective rapport.[4] Additionally, the economic burden of health conditions is significantly reduced with effective healthcare management. Therefore, this skill gap can be addressed by developing a training program that aligns with patient-centered care. Given the problem at hand, the project delivered an evidence-based curriculum product to enhance and build healthcare professionals’ skills related to encouraging positive health outcomes among their patients using MI training. Improvement in engagement skills will improve the patient’s experience and produce the desired results.
Evidence that improved care management service will then reduce the impact of chronic diseases such as cancers and asthma, which require personal self-care from the patient.[4]. The deliverables available and created in the current report have the possible advantage of the industry’s performance by explaining the skills that will improve engagement and quality patient services.[2] The intention and purpose of the deliverables in this discussion ensure that the healthcare team is educated on the skillset to support patient autonomy in changing behavior.
Methodology
The capstone project was developed to be delivered in various healthcare settings, such as hospitals or health plan settings. The target audience for this deliverable is the public health management (PHM) care management professionals. These individuals were selected within the capstone site, given their role in the organization, and interaction with patients. The project is expected to ensure improved patient and professional outcomes for the organization and participants.
Target audience: This capstone project’s target audience consisted of care managers, both medical and behavioral health clinicians, community health workers, care management service coordinators, outreach coordinators, enrollment specialists, and long-term services and support coordinators. The program may be implemented via several deliverable modes. Either in-person or in a remote, virtual environment such as ZOOM or WebEx. Providing options for instructor-led sessions allows the program to be delivered during uncertain times, such as the current coronavirus disease 2019
(COVID-19) pandemic.
Each staff member will enhance their care management practice that is reflective of MI. This enhancement in practice will impact the organization by increasing patient engagement in health coaching and disease management. Healthcare professionals will be able to guide patients in making positive changes toward improved health. The curriculum will assist in decreasing patients’ inappropriate use of medical and behavioral health services. With effective MI, a patient will experience improved satisfaction with care management services and overall engagement. Healthcare professionals will articulate and demonstrate the underlying relational component of MI, the spirit of MI, patient-centered, collaborative, and nonautocratic. Healthcare professionals will draw from MI theories and principles of engaging, focusing, evoking, and planning to support
members in care management per their healthcare discipline and field. The care management team was the target audience because they are responsible for guiding patients throughout the decision-making process about behavioral change. This team and their communication skills are important to the organization and the population served because interactions with patients determine their health outcomes.
The MI sessions will improve the care management team’s skillset in encouraging positive health outcomes by applying MI techniques intended to ease the acceptance of positive health changes for their patients. The training will build upon their patient engagement skillset. The healthcare professional will exemplify the skillset by exercising a collaborative and member-centered approach. This approach ensures that the health issues that the patient suffers from can be mitigated. This reduction is achieved through agreed-upon behavioral health changes that have been initiated and suggested by the care team. This target audience will benefit from the program by increasing the rate at which their patients act on positive behaviors to improve their health on their own.
Setting: The organization has contractual and regulatory obligations related to member decision-making documentation that reflects their own needs and preferences. For instance, insurance organizations such as chain businesses oversee health coverage for people of all age ranges with preventable diseases, whose behavioral changes would make a difference. This indicates that this project’s application improves patient outcomes and eases the healthcare professional’s role while following the care management process. Moreover, decisions would not have to be made for the patients, respecting the patient’s autonomy to make informed decisions.
Beyond the local setting: Beyond simply being healthcare professionals to the patients at the organization, the project develops skills that allow the patient-professional relationship to build further and faster. The psychosocial benefits herein will be undeniable because patients will then be more flexible and freer to talk with their care team with integrity, depending on the communication. Additionally, this eases the search for a solution. Without forcing the patient, the skills build the room for possible shared decisions from a professional to a social setting.
Ethical considerations: Ethical research and project management are critical in the capstone project. Given that the deliverable project is intended to improve organizational performance, ethical issues set forth by the institutional review board (IRB) need to be complied with. According to the IRB, central ethics entail respect for the study’s participants, which is achieved through permission and consent. Individuals supporting the capstone project’s development consist of leaders, clinical educators, and medical and behavioral health care managers. Since the project consisted of developing a training curriculum, there were no risks of potential harm to any individual. No consent forms were required per the IRB, and the capstone site stakeholders collaborated on the capstone project.
Site permission: Permissions may be given both orally and in writing. The capstone site’s quality and compliance professionals affirmed that the project was within the organization’s rules and expectations, and hence, site permissions were granted.
The project was based on the ADDIE model, consisting of five steps focusing on the first three stages: analysis, design, and development.
Analysis: The analysis phase ensured that the instructional problems were identified as well as the desired goals. The project’s objectives are developed, addressing the audience, and its characteristics, behavioral outcomes, any constraints to learning, deliverable options, and timelines were identified at this stage.[5] To analyze all constraints and learning issues, the instructional designer conducted a gap analysis by collecting both archival data and information from interviews with management. A mixed methodology was used to arrive at the root-cause analysis, and research from the literature was used to identify existing gaps (Figure 1). During this phase, a needs assessment was conducted to provide healthcare providers with the best practices to engage patients. Some of the identified ways encompassed motivational interviews and shared decision-making. The ADDIE framework’s analysis phase ensured that the project was based on the organization’s objectives and goals.
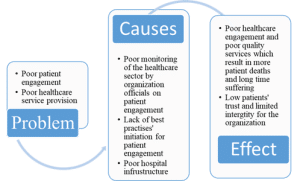
Figure 1: Root-cause map
During this phase in developing the curriculum, a needs assessment was conducted to determine the best practices healthcare providers can adopt to engage patients. Some of the identified practices encompassed motivational interviews and shared decision-making. Implementation of these strategies best enhances the interrelationships between the patients and healthcare providers, which have implications for improved care. Moreover, collaboration was essential as each team member had their input towards the project’s success.
A needs assessment is essential as it helps an organization determine the gaps that prevent it from achieving its desired goals. Similarly, a needs assessment project requires collaborative individuals to accomplish the project’s purposes.[6] This concept implies that failure to collaborate may prevent the project from achieving its goals and objectives. Nonetheless, with proper decision-making, the gaps hindering the organization from attaining its objectives were bridged. Implementation of these strategies best enhances the inter-relationships between the patients and healthcare providers. This analysis process took two weeks, engaging in interviews, questionnaire use, audio-video meetings, and case reviews.
Design: The design stage allows the instructional designer to assess the required objectives and content, develop lesson plans, and select the syllabus’ media and instruments, as well as the scope.[5] The stage gives the instructional designer the best possible learning experience for the people to educate based on the various analyses. In this stage, the instructional designer was expected to exhibit specificity and systematic application of studies into the curriculum properties. This means that the curriculum is then designed in an ordered manner, with extra attention to each detail and following all the different strategies.[1] During this phase, the instructional designer creates sections of the curriculum with attention to each section. Each section achieves strategies of key importance, and hence, the order in the guides and documents is developed.
This stage allows the instructional designer to ask key stakeholders at the capstone site more specific questions about structuring the deliverable content. Questions concerning the nature of cognitive processes expected by participants, types of knowledge and skills needed to be retained, best and most appropriate deliverable tools, and possibly, the length of each session in the deliverable can guide development. The prototype designs were made, including outlines and sections, alongside the different sessions and visual presentations designed for these purposes. The design phase is meant to be quite specific and directed. Hence, this is the stage at which the curriculum sections are created according to the objectives. The project’s policies and procedures were designed within this phase to ensure chronological order, and visual and technical design strategies (user interfaces and presentations) were aligned.
Develop: The development stage is where the contents are developed and assembled, aligned, and technologies are assigned to the different stages and sessions of the curriculum development structure. This stage allows the designer to deliver the deliverable by laying out the decided material fonts, colors, etc. The ADDIE framework allows for an iterative review and design process, and this phase is one in which the product specifications are defined further with their resources.[1] The whole process was called the input-process-output-program, with the design ensuring that feedback is achieved throughout the process, as shown in Table 1.[1] The development phase considers testing as one of the essential parts of this project to find any material and malfunction errors.[7] To ensure full testing, all the technical materials to be used within the project’s development were tested during this phase, and communication lines were tested to ensure that errors related to video conferencing and chatting features were eliminated.
| ADDIE model | Inputs | Outputs |
| Analysis | – Preliminary discussions with personalized recovery-oriented service program providers, recipients, and the Office of Mental Health staff | – Learning needs data – Pilot curriculum and training program – Revised learning objectives and format to scale training |
| Design | – Learning objectives, development of evaluation, and media selection – SME and module development team of the design document |
– Design document – Revised design document |
| Development | – Authoring tool applied to design documents to develop multimedia training – Module development and learning management system team review of the module |
– Multimedia e-learning module |
Table 1: Input-process-output
Project outcomes: The deliverable is a comprehensive MI training curriculum consisting of two components: a facilitator’s guide and a participant’s guide. The first component developed was the MI facilitator’s guide. A facilitator’s guide contains all the necessary resources to deliver instructor-led and hybrid deliverables. Facilitators will have a menu of options to select from as it relates to in-person workshops and practicums. The facilitator’s guide is created with a possible reflection of all nine events of instruction as proposed by Miner et al.[8] gaining attention, informing the learners of the objectives, stimulating recall of prior learning, presenting the stimulus, providing the learning guidance, and eliciting performance with examples in table 2. These instructional strategies ensure that the deliverable is efficient in systematically delivering the skillset required. The guide and the skills it imparts, according to Bershad et al.[9] can create and strengthen professionals’ commitment to the program.
| Events of instruction | Activity | Examples |
| Gain attention | Introductory mass email; Introductions; Level set the importance of the program | Introductory slide in the computer-based training module; video or skit |
| Inform learner of objectives | Objectives for the program are disseminated | Objective slide, page in manual, part of description in learning management system (LMS) |
| Stimulate recall of prior learning | A general overview of high-level concepts will be delivered | Examples (fill in the blank), engaging prior experience or knowledge in the program topic/focus |
| Present stimulus | Deliver content | The program modules |
| Provide learner guidance | Provide learners with an exam | In-course examples, scripts, scenarios, etc. |
| Elicit performance | Give learners practice activities | In-course examples, case studies, role-play, etc. |
| Provide feedback | Immediate, specific, correct, and relevant feedback to learners | Pop-ups, feedback slides, markers, etc. |
| Assess performance | Learners complete a knowledge check/quiz/exam | Minimal scores required for each module; each module requires a passing score to achieve program completion |
| Enhance retention and transfer | Provide resources, job aids, and tools; Encourage department support | Appoint department champions/leads; open-door training policy; peer-to-peer resource |
Table 2: Events of instruction
The facilitator’s guide enables instructors to use outlined lessons to teach MI fundamentals and utilize patient-centered counseling skills. Additionally, the guide seeks to equip facilitators with the knowledge to ensure that participants can attain the course objectives and change to healthy behaviors through their education. Therefore, the guide consists of five skill tasks to be followed by instructors: the spirit of MI, engaging, focusing, evoking, and planning. According to Schoo et al.[10] The study of these skills is significant to the organization. The second component developed is the core of the curriculum, the participant guide, consisting of five lessons aligned with the designed facilitator’s guide to ensure that all five lessons are delivered. Lesson one of the participant guides aligns sub-modules relating to covering the spirit of MI and MI’s history. For the learners, the lessons allow for self-reflection, which according to Schoo et al.[10] They are very beneficial alongside feedback to ensure that they are embedded. Souza et al.[11] confirmed that guides instructing the coaches or facilitators could resolve ambivalence, increase patient-centered care, and allow quick implementation regardless of the organization’s busy schedules.
Development process: The process was initiated through communication and analysis of stakeholders. The organization, respectively, followed with data collection through procedures indicated in table 3. Information gathered–interview responses, audio-visual meetings, questionnaires, and group replies–was further analyzed. Thematic analyses also discussed the problem, and these were complemented with root-cause, gap, and contextual analyses to understand the problem and identify the organization’s gap. This process was followed using literature to understand the background of the issue and a possible solution through mixed research methods.
| Type of Information | What the researcher requires | Method |
| Contextual | Organizational background, history, and structure; mission; vision; values; products; services; organizational culture; leadership; staff and site description | Document review, observation |
| Demographic | Descriptive information regarding participants, such as age, gender, ethnicity, discipline, etc. | Survey |
| Perceptual | Participants’ descriptions and explanations of their experiences as they relate to the phenomenon under study | — |
| Research question | Write out what you specifically want to know regarding this question. | Interview, critical incidents, focus group |
Table 3: Summary of qualitative methods for primary data collection
Following this, the organization’s leadership provided permission to develop the curriculum, followed by input from key stakeholders, for example, clinical educators, medical and behavioral health care managers who showed interest in taking part in the project. This permission also provided the necessary authority to access and review case files. The capstone site group frequently met to discuss the capstone project’s progress, specific recommendations made by the school, and the instructional designer’s mentor. At the initial roll-out meeting with key stakeholders, the instructional designer set expectations for how the group would collaborate and when feedback would be necessary. This feedback would be used to emendate the capstone project as appropriate. The capstone site team, outside of the instructional designer’s capstone work, met on a biweekly basis.
The capstone site team determined what topics were most appropriate and relevant to healthcare management services as a group. The determination resulted in a program consisting of five lessons addressing the skills of MI. The five lessons addressed the MI components of MI’s spirit, engaging, focusing, evoking, and planning. Using the ADDIE model to identify and align the problem with the solution through a five-step process: analyzing, designing, developing, implementing, and evaluating, the instructional designer developed a deliverable made for the instructor and participant, showing the desired skills to be trained to the organization’s staff. Following the facilitator guide, which included engaging, focusing, evoking, and planning, a participant guide was designed to follow these skills to fit the MI training skills. Through the capstone project framework, adult learning theories have been embraced to ease the delivery of these skills to the professionals, given that all are adults. Through this guidance, the deliverable is aligned with the organization.
Evaluation plan: The Kirkpatrick model provides some guidance on how best to measure the effectiveness of training, and this model has been chosen for the evaluation plan to enable the organization’s decision-makers to review the product or training schedule before it is fully incorporated into the organization’s training schedule.[12] One of the most common ways the decision-makers will evaluate such a product is by surveying participants after they complete a pilot session. They could ask questions to gather employee feedback, whether through a formal or informal training evaluation questionnaire. The Kirkpatrick Model aligns evaluation in three different levels: reaction, learning, and behavior.
Level 1: The first level of evaluation would gauge the reaction of the employees. The first level, therefore, evaluates how satisfied or engaged the employees were with their training. The level also assesses how relevant they feel that the training is to their roles and duties.[13] Were you satisfied with the overall training?
- Did the training exercise an effective and satisfying use of your time? Would you classify it as being disruptive?
- Can you recommend this training for any other professionals?
- Has the training been able to enlighten your knowledge and grow your desire to take on a particular career change or improvement goal in your life?
Level 2: The second evaluation level involves measuring how well the participants attained the materials based on their skills, knowledge, attitudes, commitment, and confidence. This phase involves some of the other evaluation methods to be more effective, such as using tests and quizzes.[14] The following questions were developed to assess the participants’ level of learning:
- Do you believe that you have gained the skills you are required to learn?
- How could you rate the knowledge you gained based on the concepts used on a scale of one to ten?
- Are there any specific topics developed in the training that you have not understood?
- Has the organization made some of these topics more relevant or less important for you?
- Would you be specific about which topics you feel are more irrelevant and why?
Level 3: The third evaluation level pertains to behavior and assesses the practicality of the training. It checks how well the participants can apply what they learned when they are trained for their jobs. The Kirkpatrick model states that incentives and encouragement from leadership are needed for this stage to be a success.[15] The following questions are developed to evaluate the team’s behavior:
- Are you making use of what you learned in your daily work duties?
- Are there any visible improvements in the team and individual performance?
- What are the characteristics within the work environment that the employee can use to apply what they have learned?
- Are there any visible changes in the way the employees coordinate or communicate?
Results
The most immediate outcome will be understanding the curriculum by the learners, which is the utmost start of change. Followed by this outcome are practice and retention, among other outcomes and findings. Healthcare professionals will draw from MI theories and principles of MI’s spirit, engaging, focusing, evoking, and planning to support care management for patients.
Short-term outcomes and findings: Participants will complete the different modules of the curriculum and demonstrate the knowledge and skills obtained.
After lesson 1, the learners will be able to:
- Describe why MI is an important skill for care management at the organization
- Define MI at the laymen, technical, and clinical levels
- Articulate the historical development of the MI framework
- Articulate and demonstrate the spirit of MI
- Explain the dual-expertise model
- Explain the patient-centered model of care by Carl Rodgers
- Explain the four strategies to MI: empathy, self-efficacy, resistance, and discrepancy
After lesson 2, full participation of the health care management team will ensure the ability of participants to:
- Define engagement per the MI framework
- Identify and recognize the righting reflex
- Articulate member engagement and disengagement
- Articulate and demonstrate the core interviewing skills: open-ended questions, affirmations, reflective listening, and summaries
After lesson 3, because of the full participation of the health care management team, the participants will:
- Define focusing on the MI framework
- Identify and articulate the three focusing scenarios: clear direction, choices in direction, unclear direction
- Demonstrate how to develop SMART goals
- Articulate the information exchange strategy of Elicit-Provide-Elicit. After lesson 4, the full participation of the health care management team will ensure that the participants can:
- Define focusing, change talk, and sustain talk per the MI framework
- Identify member change talk and sustain talk • Articulate how to handle sustain talk
- Articulate the practical use of the readiness ruler
After lesson 5, the full implementation of the curriculum will ensure that the different learners and hence participants can:
- Identify member readiness for change
- Develop a change plan for member readiness
- Consolidate commitment through strengthening member commitment and supporting change
These are the most immediate steps of taking on the curriculum based on completing the deliverable. The achievement of these outcomes by participants will improve the skillset of the healthcare provider as they interact with the patients with whom they engage.
Mid-term outcomes: Mid-term outcomes will require the practice and observation of the healthcare professionals involved in the training. Once the capstone site implements the training, healthcare professionals will articulate and demonstrate the underlying relational component of MI – the Spirit of MI, patient-centeredness, collaboration, and nonautocratic.[2] Based on their healthcare discipline and field, professionals will apply MI theories and the principles of engaging, focusing, evoking, and planning to support care management team members. Through their communications and relationships with one another and patients within the following period, approximately two months, it is expected that healthcare professionals can engage patients and evoke the kind of positive motivation among patients to take on self-management more appropriately.
Project outcomes include developing a robust training curriculum to close the gap in skillset regarding patient engagement successfully. Each staff member will enhance their care management practice that is reflective of MI. The practice of what has been taught will be viewed through the program’s mid-term evaluation by the leaders based on the improvements within the different employee performance sections.
Long-term outcomes and findings: Long-term outcomes are evidenced in the literature on the importance of MI being administered in line with the different modes of education and theories. According to the literature, this enhancement in practice will impact the organization by increasing patient engagement in health coaching and disease management.[3] Organizational improvement will start with the healthcare professionals’ training in MI, and as they put into action and practice what they have learned. Ultimately, it is expected that this will improve their care management characteristics, as revealed in the relevant literature.
Discussion
Patient engagement, as initiated by the clinicians, has been proven to impact patient outcomes and their attitude towards the reception of advice on personal behavior. Bombard et al.[16] confirmed that most studies find that patients’ level of engagement determines their behavioral change and adherence to healthcare recommendations. Care processes and service deliverables hold a vital position in patient outcomes overall. Additionally, Bombard et al. found that patients who feel less involved in the decisions made for their lives were less likely to adjust to change, especially if suggestions were rejected.
Thematic analyses and systematic review by Albury et al.[17] discovered that most patients are angered by the mention of the relationship between their health condition and their behavior unless the communication is calmly initiated by the professional with techniques such as focusing on patient-initiated topics, collaboration, and ensuring open-ended discussions that are not restrictive. For these reasons, the need to understand MI is important if healthcare management professionals are to influence their patients’ actions.
The capstone project solves an organizational concern that indicates a lack of adequate care management skills regarding MI.[3] MI has been applied in the healthcare sector for approximately two decades now. Its evolution started from the Rogerian patient-centered approach, which was ameliorated with different theories to guide behavioral change influenced by collaboration with the patient.[18] In opposition to medical direction and imposition, the MI approach embraces patient autonomy and overall self-efficacy. In that, the patient can apply the available resources to personal decision-making to improve their circumstance rather than rely upon expert evidence and instruction. The literature further indicates that the use of MI enhances communication with patients and strengthens patient-professional relationships. It can also support desired patient outcomes, enabling the patient to choose safer behavior without being forced to act by a healthcare professional, preferably through mutual agreements.[2]
According to Scott et al.[18] a healthcare team’s MI communication skills to improve patient outcomes are active listening, reflection, and open-ended questions that allow for elaboration. Improved patient outcomes in combination with improved organizational results are something all organizations desire. Consideration of methodologies to apply to each step of the project was dependent on the nature of the information required. Mixed methods—qualitative and quantitative methods, alongside the use of both the secondary and primary sources, are justifiably vital because they allow qualitative data to complement any quantitative data presented.[19]
The needs assessments used qualitative interviews with first-hand information to respond fully with emotions and reactions monitored. This, as preliminary information, is enhanced with secondary data from sources to show the literature gap and analysis.[20] Additionally, the methods in this report are justified by Regnault et al.[19] who noted that the use of all these methods has ensured improved innovative outcomes in healthcare management through the consistent use of data.
While studies regarding the improvements in health conditions and self-management of diseases show that patient motivation is a factor, persistence in the results has been contested. Dorstyn et al.[21] noted that most randomized controlled trials indicate that MI’s application can influence behavioral, mental, psychological, and social changes among patients with multiple sclerosis. Additionally, Li et al.[22] argued that the same had been noted with patients dealing with diabetes, resulting in their proper management of total cholesterol, fasting blood glucose, body mass index, blood pressure, waist circumference, and physical activity.
According to Scott et al.[18] MI takes on a “direction” style accompanied by an element of “following,” which causes the patient to sense guiding cognitively but not leadership or command, and hence the willingness and feeling that they have been given the autonomy to decide. Additionally, Frost et al.[23] noted that MI’s application had been found to control binge drinking behaviors, control the frequency and quantity of alcohol consumption, substance abuse in people with dependency or addiction, and increase physical activity participation. However, these studies indicate that the sustainability of these behavioral changes and continuity of these benefits are hardly evident or under-researched. Moreover, MI’s application and efficiency depend not only on the nature and style of teaching but also on the organizational response to change. Also, MI’s effectiveness has hardly been quantified, given that behavioral change is timely and limited, while it is based on other factors.[21]
Most of the literature has explored the benefits that have been related to the impact of MI. The following examples show that the study made use of literature about systematic reviews on diseases. Dorstyn et al.[21] assessed ten randomized controlled trials to create a systematic review of pooled results that indicated that MI, hand in hand with counseling or rehabilitation techniques, caused significant improvements, medium to high significance in the social, psychological, and behavioral outcomes. However, the assessment noted that MI results were rarely researched, with less frequency, and that the results are likely to last a maximum of seven months. According to Dorstyn et al.[21] all the intervention delivery modes were proven effective.
Similarly, Bombard et al. and Albury et al.[16,17] presented studies using systematic reviews and thematic analyses that take on different stakeholders: patients and educators, respectively. Bombard et al.[16] used a thematic analysis that checks the strategies and contextual factors that enable optimal patient engagement, patient engagement outcomes, and patients’ experiences of being engaged. Different approaches were grouped based on design, development, leadership, and recruitment, among other criteria. The patient’s levels of engagement and outcomes based on MI were analyzed, and so were the negative ones related to the patient’s emotions and feelings, which were excluded from their decision. Albury et al.[17] used conversational studies and discourse analysis studies to assess physicians and their patients’ communications. The analysis notes that communication modes and initiation of the behavioral change topic with patients were based on their relationship and initiation. The study elucidates why the medical team needs to be educated on the patients’ motivational interviewing role and ability.
Scott et al.[18] explored how nurses can apply MI to ensure and encourage patients to take on behavior change. The analysis explained the different principles upon which MI relies and the proven examples of MI’s prolonged application in the healthcare sector. Furthermore, the study underpins MI as one of the most efficient and effective in solving the National Health Service medical productivity issues in the United Kingdom. As evidence, Scott’s study elucidates that the intervention is effective in behavioral change. Szczekala et al.[2] used the Motivational Interviewing Treatment Integrity (MITI) scale in a set of countries to assess the effectiveness of MI’s application. The study used the tool to measure motivational training’s competence, consequently applying this to determine the available MI and benefits to both the patients and professionals. Through a non-systematic literature review from 2005 to 2018, the study analyses PubMed on the intervention’s efficiency across these countries. The study found that patients are encouraged to check their behavior when approached with the knowledge and understanding of their health condition and personal roles in their lives. The study also found that healthcare professionals can gain better communication skills, self-confidence, professionalism, and increased morale through exercising MI.
Frost et al.[23] performed a systematic review that considers the impact and effectiveness of MI for society concerning behavioral change. A set of seven databases, Cochrane Database of Systematic Reviews (CDSR), Database of Abstracts of Reviews of Effects (DARE), International Prospective Register of Systematic Reviews (PROSPERO), Medical Literature Analysis and Retrieval System Online (MEDLINE), Cumulative Index to Nursing and Allied Health Literature (CINAHL), Allied and Complementary Medicine Database (AMED), and Psychological Information Database (PsycINFO) from 2000 to May 2018, were selected for the study to deliver a quantitative assessment of the effectiveness of the intervention.
According to the results, seven percent of the meta-analyses show that the change lasts approximately six months with excellent results of reduced eating disorders, alcohol and drug consumption, and improved physical activity for different patients. According to Szczekala et al.[2], MI training and experience for professionals benefit the patients and the organization and improve self-efficacy among patients. Additionally, this means that patients can manage their care with an improved sense of self-motivation and satisfaction. Following this, healthcare professionals’ satisfaction and performance are key to long-term outcomes that are to be expected with the implementation of an MI training program. With this purpose, about individual healthcare professionals’ performance, they will be enabled to guide patients towards positive behavior choices better.
The curriculum will help decrease patients’ inappropriate use of medical and behavioral health services.[4] For instance, MI enables improved patient outcomes in the mental health field by educating the teams on how to teach patients to visualize their futures without any substance abuse or mental struggles. MI also helps individuals realize the need to change independently by allowing patients to talk through their problems and convincing them to take their medications as prescribed.[24] Furthermore, evidence concerning diabetes and multiple sclerosis reveals that using MI techniques allows for flexibility for the professionals to approach the patients in a collaborative way to improve self-care with lasting benefits and behavioral change.[21,22] With effective MI, patients will experience improved satisfaction with care management services and overall engagement.
Implications for professional specialization: The application of the instructional designer’s project soars beyond merely educating individuals on these skills but delves deeper into a goal that all healthcare professionals seek and practice: patient-centered care. Having this nature of the relationship and skill pertaining to the care management teams also improves the ability to learn from one another in improving patient and organizational outcomes.
Recommendations: The capstone project is focused on care management teams, given that they are more in contact with patients. However, MI is a skill set that should be and can be pursued by all professionals in healthcare because, at one point, all individuals must face a patient. Moreover, autonomy, being a nursing ethic, is important for all healthcare professionals, and patient outcomes are also important. Both rely on the patient’s willingness to take on behavioral change, which can be advised but not forced. As such, MI is important in all healthcare fields. The instructional designer recommends that organizations not selectively apply education sessions to specific staff members but rather educate all people within the organization. Education on MI improves the patient’s health outcomes and, in turn, ensures that the organizational performance improves through the prevention of re-admissions and unnecessary, costly services.
Further recommendations are that the application and implementation of the MI sessions as per the curriculum be further developed to fit the different organizational structures and changes to improve education consistency. Training and development sessions can be used to delve into the healthcare professionals’ education on MI, which would ultimately mean that the frequency of education on MI will increase. Consistent education on MI’s qualities and features will provide the organization and professionals with the opportunity to practice and make these practices a part of their day-to-day operations. The approach towards putting in best practices should always involve physicians’ opinions and patients’ opinions rather than being dictated by the organization. The healthcare sector is continuously evolving in terms of technology and skill development. The deliverable can be made more flexible based on the organization’s nature, population, and other considerations. In this light, the instructional designer suggests that the implementation and use of technology should be involved in creating models that can focus on the populations served. It may be beneficial to guide more direct frameworks on the types of populations and conditions experienced to make the sessions more realistic. Technology will improve communication, reach those who may not attend an in-person event, and ensure the training is accessible to all.
The integration of the developed curriculum on MI in an organization aligns with the organization’s culture. Organizations can ensure consistent education by making organizational training and development part of the organizational structure and culture to ensure that the professionals are knowledgeable. However, continued development and updating of the curricula and skills should be done as an organizational task, including this capstone product, to benefit the organization based on desired results. The curriculum should be developed by an informed team to ensure that it is updated whenever needed after a committee decides on program enhancements. In this sense, the organizations can have a repository of MI curriculum and training that benefits the organization in meeting the needs of the population served.
Conclusion
The capstone project developed a curriculum product to improve healthcare professionals’ skill sets and encourage positive health outcomes through MI training. The problem is the gap in healthcare professionals’ skillset in helping patients address and manage physical health conditions such as addiction, diabetes, heart disease, and asthma. Therefore, the project’s purpose was to deliver an evidence-based curriculum product that would enhance and build healthcare professionals’ skills in encouraging favorable health outcomes among their patients using MI training. The capstone project’s curriculum model and design steps followed the ADDIE model to develop a course in steps: analysis, design, development, implementation, and evaluation. The deliverable consists of a facilitator’s guide with a menu of options for
in-person sessions containing suggested lesson plans, notes, handouts, resources, and course assessments. A participant’s guide was also created and can be issued directly to participants or made available on a platform. Participants can download this guide directly to support a virtual/remote deliverable when necessary.
The most important outcome has been the development of the curriculum to support professional development. The deliverable is intended to develop MI skills that can be used to support patients interactively and change their behavior willingly. Professional communication skills from healthcare professionals allow patients to make personal decisions on behavioral changes to improve their health through positive interactions. Healthcare professionals who engage in the program herein will have the ability to influence their patients’ behavior and support their patients’ self-efficacy in caring for themselves. As an organization, favorable patient outcomes are the most important, and improvement in patient engagement will support this goal.
References
- Nichols Hess A, Greer K. Designing for engagement: Using the ADDIE model to integrate high-impact practices into an online information literacy course. Comminfolit. 2016;10(2):264. doi:10.15760/comminfolit.2016.10.2.27 Crossref | Google Scholar
- Szczekala K, Wiktor K, Kanadys K, Wiktor H. Benefits of motivational interviewing application for patients and healthcare professionals. Pol J Public Health. 2018;128(4):170-173. doi:10.2478/pjph-2018-0034 Crossref | Google Scholar
- Lim D, Schoo A, Lawn S, Litt J. Embedding and sustaining motivational interviewing in clinical environments: a concurrent iterative mixed methods study. BMC Med Educ. 2019;19(1). doi:10.1186/s12909-019-1606-yPubMed | Crossref | Google Scholar
- Dineen-Griffin S, Garcia-Cardenas V, Williams K, Benrimoj SI. Helping patients help themselves: A systematic review of self-management support strategies in primary health care practice. PLoS One. 2019;14(8):e0220116. doi:10.1371/journal.pone.0220116 PubMed | Crossref | Google Scholar
- Patel SR, Margolies PJ, Covell NH, Lipscomb C, Dixon LB. Using instructional design, analyze, design, develop, implement, and evaluate, to develop e-learning modules to disseminate supported employment for community behavioral health treatment programs in New York State. Front Public Health. 2018;6. doi:10.3389/fpubh.2018.00113 PubMed | Crossref | Google Scholar
- Schirmer JM, Cartwright C, Montegut AJ, Dreher GK, Stovall J. A collaborative needs assessment and work plan in behavioral medicine curriculum development in Vietnam. Fam Syst Health. 2004;22(4):410-418. doi:10.1037/1091-7527.22.4.410 Crossref | Google Scholar
- Culatta R, Culatta B, Frost M, Buzzell K. Project SEEL: Part II. Using technology to enhance early literacy instruction in Spanish. J Spec Educ Tech. 2004;19(2):89-96. doi:10.1177/15257401040250020601 Crossref | Google Scholar
- Miner A, Mallow J, Theeke L, Barnes E. Using Gagne’s 9 Events of Instruction to enhance student performance and course evaluations in undergraduate nursing courses. Nurse Educ. 2015;40(3):152-154. doi:10.1097/nne.0000000000000138 PubMed | Crossref | Google Scholar
- Bershad D. Motivational interviewing: A communication best practice. American Nurses Association. 2019. Motivational interviewing: A communication best practice
- Schoo MA, Lawn S, Rudnik E, Litt CJ. Teaching health science students foundation motivational interviewing skills: use of motivational interviewing, treatment integrity, and self-reflection to approach transformative learning. BMC Med Educ. 2015;15(1). doi:10.1186/s12909-015-0512-1 PubMed | Crossref | Google Scholar
- Souza AM. Introducing the health coach method of motivational interviewing to medical assistants to improve the patient care approach. Dissertation. Walden University; 2017. Introducing the Health Coach Method of Motivational Interviewing to Medical Assistants to Improve the Patient Care Approach
- Kirkpatrick JD, Kirkpatrick WK. Kirkpatrick’s Four Levels of Training Evaluation. Association for Talent Development; 2016. Kirkpatrick’s Four Levels of Training Evaluation
- Moreau KA. Has the new Kirkpatrick generation built a better hammer for our evaluation toolbox? Med Teach. 2017;1-3. doi:10.1080/0142159x.2017.1337874 PubMed | Crossref | Google Scholar
- Jones C, Fraser J, Randall S. The evaluation of a home-based paediatric nursing service: concept and design development using the Kirkpatrick model. J Res Nurs. 2018;23(6):492-501. doi:10.1177/1744987118786019 PubMed | Crossref | Google Scholar
- Agarwal N, Pande N, Ahuja V. Expanding the Kirkpatrick evaluation model towards more efficient training in the IT sector. Int J Hum Capital Inf Technol Prof. 2014;5(4):19-34. doi:10.4018/ijhcitp.2014100102 Crossref | Google Scholar
- Bombard Y, Baker GR, Orlando E, et al. Engaging patients to improve quality of care: a systematic review. Implement Sci. 2018;13(1). doi:10.1186/s13012-018-0784-z PubMed | Crossref | Google Scholar
- Albury C, Hall A, Syed A, et al. Communication practices for delivering health behaviour change conversations in primary care: a systematic review and thematic synthesis. BMC Fam Pract. 2019;20(1). doi:10.1186/s12875-019-0992-x PubMed | Crossref | Google Scholar
- Scott G. Motivational interviewing 1: background, principles and application in healthcare. Nurs Times. 2010;106(34):21-22. Motivational interviewing 1: background, principles and application in healthcare
- Regnault A, Willgoss T, Barbic S. Towards the use of mixed methods inquiry as best practice in health outcomes research. J Patient Rep Outcomes. 2018;2(1):19. doi:10.1186/s41687-018-0043-8 PubMed | Crossref | Google Scholar
- Segal C. Misbehavior, education, and labor market outcomes. J Eur Econ Assoc. 2013;11(4):743–779. doi:10.1111/jeea.12025 Crossref | Google Scholar
- Dorstyn DS, Mathias JL, Bombardier CH, Osborn AJ. Motivational interviewing to promote health outcomes and behaviour change in multiple sclerosis: a systematic review. Clin Rehabil. 2020;34(3):299-309. doi:10.1177/0269215519895790 PubMed | Crossref | Google Scholar
- Li Z, Chen Q, Yan J, Liang W, Wong WCW. Effectiveness of motivational interviewing on improving Care for Patients with type 2 diabetes in China: A randomized controlled trial. BMC Health Serv Res. 2020;20(1):57. doi:10.1186/s12913-019-4776-8 PubMed | Crossref | Google Scholar
- Frost H, Campbell P, Maxwell M, O’Carroll RE, Dombrowski SU, Williams B, Cheyne H, Coles E, Pollock A. Effectiveness of motivational interviewing on adult behaviour change in health and social care settings: A systematic review of reviews. PLoS One. 2018;13(10):e0204890. doi:10.1371/journal.pone.0204890 PubMed | Crossref | Google Scholar
- Alyssa B. How Motivational Interviewing Can Treat Mental Illness? Banyan Mental Health. Published June 1, 2018. Accessed April 28, 2025. How Motivational Interviewing is Beneficial | Banyan Mental Health
Acknowledgments
I would like to express my gratitude to my manager, Melissa Major, for her guidance, support, and sponsorship throughout each stage of my doctoral capstone. The training, quality, and compliance team is truly fortunate to have such an honest, bold, and positive leader. I also want to thank my mentor, Dr. Edna Waller. Her flexibility and willingness to support me have been exceptional, and I deeply appreciate her time and guidance over the past two terms. Lastly, I would like to thank my professor, Dr. Kathryn Jones. Her positivity and expertise played a crucial role in maintaining momentum throughout the program, and her support with the initial proposal was unparalleled.
Funding
The instructional designer is not receiving payment for the development of the curriculum product.
Author Information
Angel Daniel Giles
Department of Education
Capella University, USA
Email: angel@healthguardcpr.com
Authors Contributions
The author contributed to the conceptualization, investigation, and data curation by acquiring and critically reviewing the selected articles and was involved in the writing – original draft preparation and writing – review & editing to refine the manuscript.
Ethical Approval
Ethical research and project management are essential to the capstone project, which aims to enhance organizational performance. In line with IRB guidelines, respect for participants was ensured through necessary permissions. As the project involved developing a training curriculum with no risk of harm, consent forms were not required. Leaders, clinical educators, and healthcare managers supported and collaborated on the project.
Conflict of Interest Statement
A conflict of interest in this project could arise if the instructional designer were to receive financial gain, a promotion, or other compensation for creating the product. Because the designer is involved in both the project and the organization, this dual role presents a potential conflict. To mitigate this risk, the designer collaborated closely with other stakeholders.
Guarantor
None
DOI
Cite this Article
Angel DG. Enhancing Patient Engagement: A Motivational Interviewing Curriculum for Health Care Providers. medtigo J Med. 2025;3(2):e30623213. doi:10.63096/medtigo30623213 Crossref






