Author Affiliations
Abstract
The study aimed to simulate and analyze a suitable antenna operating at an optimized frequency for microwave ablation of breast cancerous tissue. Four different antennas were simulated and analyzed using finite element method (FEM) software. Based on the variation in their reflection coefficient, total power density, and Specific Absorption Ratio, three of the antennas were selected. The four antennas have different geometry parameters based on the effective wavelength in breast tissue at the variable frequencies. Power loss for all simulated microwave antennas was above 50% from an input power of 10 W. The simulated single slot antenna proved efficient but had high power dissipation. The simulated monopole antenna with a radiating length of 8 mm performed better than the other monopole antennas. Among the frequencies tested, 6.02 GHz had the lowest reflection coefficient but high-power dissipation. Considering power dissipation, backward heating along the antenna shaft, and aspect ratio of necrotic tissue, the simulated monopole antenna with an 8 mm radiating length operating at 6.61 GHz was found to be the most efficient.
Keywords
Radiofrequency ablation, Microwave ablation, Breast ablation, Relative permittivity, Reflection coefficient, Thermal conductivity.
Introduction
Breast cancer is the predominant form of cancer affecting women worldwide, constituting approximately 23% of all newly diagnosed female cancers in over 1.1 million women annually.[1] Tragically, breast cancer claims the lives of more than 411,000 women each year, accounting for over 1.6% of all female deaths caused by various factors. Additionally, female breast cancer amounts for 11.7% of recently diagnosed cancers and 6.9% of advanced-stage cancers.[2,3]
Microwave ablation is the treatment that uses high temperatures to heat up body tissue, damaging and killing cancer cells, or to make cancer cells more sensitive to the effects of radiation and certain anticancer drugs.[2,4,5] Existing systems use low-frequency ranges like 915 MHz or 2.45 GHz, requiring high microwave power, leading to increased equipment size, cost, and backward heating risks.[6] Common antennas used in microwave cancer therapy include monopole, dipole, and slot.[7] Moreover, because of the self-heating of the applicator by the excessive microwave power, additional means for cooling are necessary to avoid harming healthy tissues; as such, suitable frequencies can help address the limitations of microwave ablation in breast cancer management.
Computational modeling enables evaluation of internal electric fields, currents, and energy deposition in the context of electromotive force (EMF)-human body interaction.[8] It uses Maxwell’s equations to obtain solutions and provides data on the average specific absorption ratio (SAR). Studies on computer modeling and simulations have contributed to research on microwave ablation of cancerous tissues.[9-11]
Material properties of biological tissues, such as permittivity and conductivity, determine how microwaves interact with the body. Tissue permittivity is affected by temperature and moisture. Dielectric properties of tissues vary with frequency, temperature, and moisture content. Breast tissue has low moisture content, resulting in low permittivity and conductivity. Commonly used microwave frequencies (915 MHz and 2.45 GHz) may not provide optimal coagulation in breast tissue. Choosing a suitable antenna operating at an optimized frequency is crucial for achieving a better coagulation zone with minimal damage to surrounding healthy tissues.
Methodology
In this study, the FEM (COMSOL MultiphysicsTM version 4.4) was used to model the electromagnetic field and for the computation of the temperature field, radiation field, Specific Absorption Ratio and temperature distribution using the bioheat equation. ImageJ was used to determine the dimensions (such as diameter, length, and aspect ratio) of the necrotic (ablation zone) breast tissue. The single-slot and monopole microwave antennas used in this study are. It is composed of inner and outer conductors, a dielectric between them, and a catheter that is made of polytetrafluorethylene (PTFE).[12,13] The catheter allows physical protection of the antenna and improves the electromagnetic coupling between the antenna and the fat tissue. The dimensions of the single slot microwave coaxial antenna (MCA) and monopole antenna are shown in Table 1.
| Antenna materials/Dimensions | ||
| Materials | Dimensions (mm) – Single slot | Dimensions (mm) – Monopole |
| Inner conductor | 0.256 | 0.252 |
| Dielectric | 0.582 | 0.582 |
| Outer conductor | 0.262 | 2.262 |
| Catheter | 0.2 | 0.2 |
| Slot | 0.262, height = 2 mm | 0.262, height = varied |
Table 1: Antenna materials/Dimensions and tissue properties
The breast tissue (breast fat) is modeled in a cylindrical form, and its material is uniform. The dimension of the tissue is 30 mm in large and 90 mm in depth. The antennas were inserted in the breast tissue at an insertion depth of 70 mm. The relative permittivity and the conductivity of the fat vary with frequency. These values, together with antenna characteristics, are given in Table 2.
| Parameters | Abbreviations | Values |
| Density of blood | ρ_blood | 103(kg/m3) |
| Specific heat, blood | Cp_blood | 3639(J/(kgK) |
| Blood perfusion rate | ω_blood | 3.6 x 10-3(1/s) |
| Blood temperature | T_blood | 37(℃) |
| Relative permittivity, fat (at different frequencies) | ε_fat | 14 |
| Electric conductivity, fat (at different frequencies) | σ_fat | 14(s/ms/m) |
| Thermal conductivity, fat | k_fat | 0.21(W/(m·K)) |
| Relative permittivity, dielectric | ε_diel | 2.03 |
| Relative permittivity, catheter | ε_cat | 2.6 |
| Microwave frequency | f | Varied |
| Input microwave power | P_in | 10(W) |
| Time | T | 300(s) |
The software’s radiofrequency and heat modules were utilized to simulate the electromagnetic interaction described by Maxwell’s equations between the electromagnetic field and biological tissue, as well as the subsequent thermal effects governed by Pennes’ bioheat equation.[14,15]
Results & Discussion
A total number of 26 simulations were made based on the frequency range (i.e., 0.03 GHz – 9.22 GHz with an approximate interval of 300 MHz). The results for the selected simulated frequencies and the antenna types using a microwave power of 10W and a heating time of 300 s are presented in Figures 1-11 and Table 3.
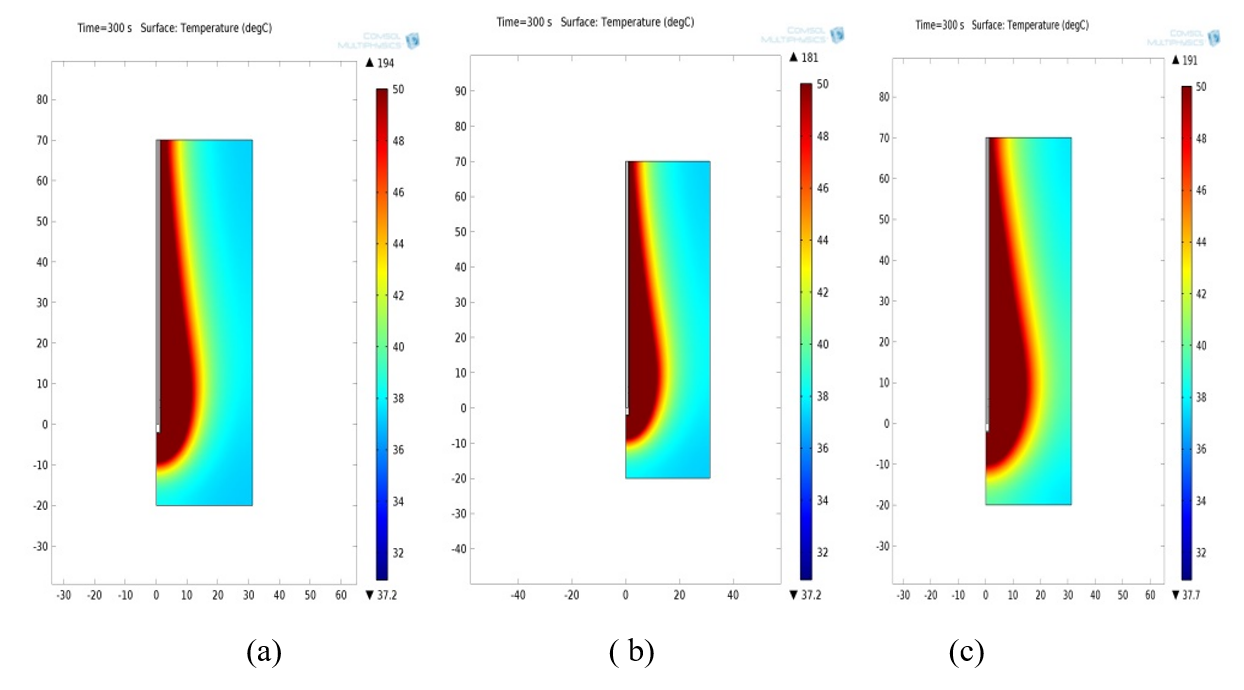
Figure 1: Temperature distributions using a single slot antenna at a microwave power input of 10 W. The isotherm at 50 ºC is highlighted. (a) at 2.72GHz (b) at 3.59GHz (c) at 4.47GHz
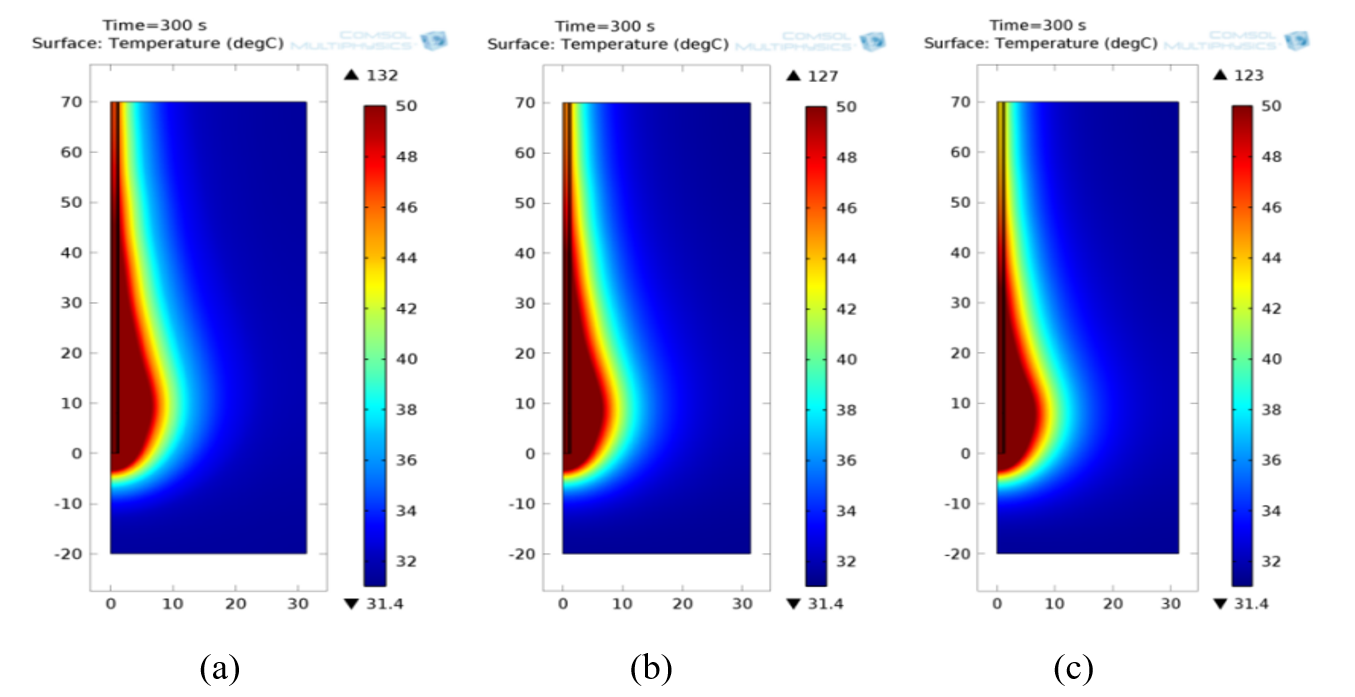
Figure 2: Temperature distributions using a monopole antenna with a radiating length of 8mm at a microwave power input of 10 W. The isotherm at 50 ºC is highlighted. (a) at 5.44GHz (b) at 6.02GHz (c) at 6.61GHz
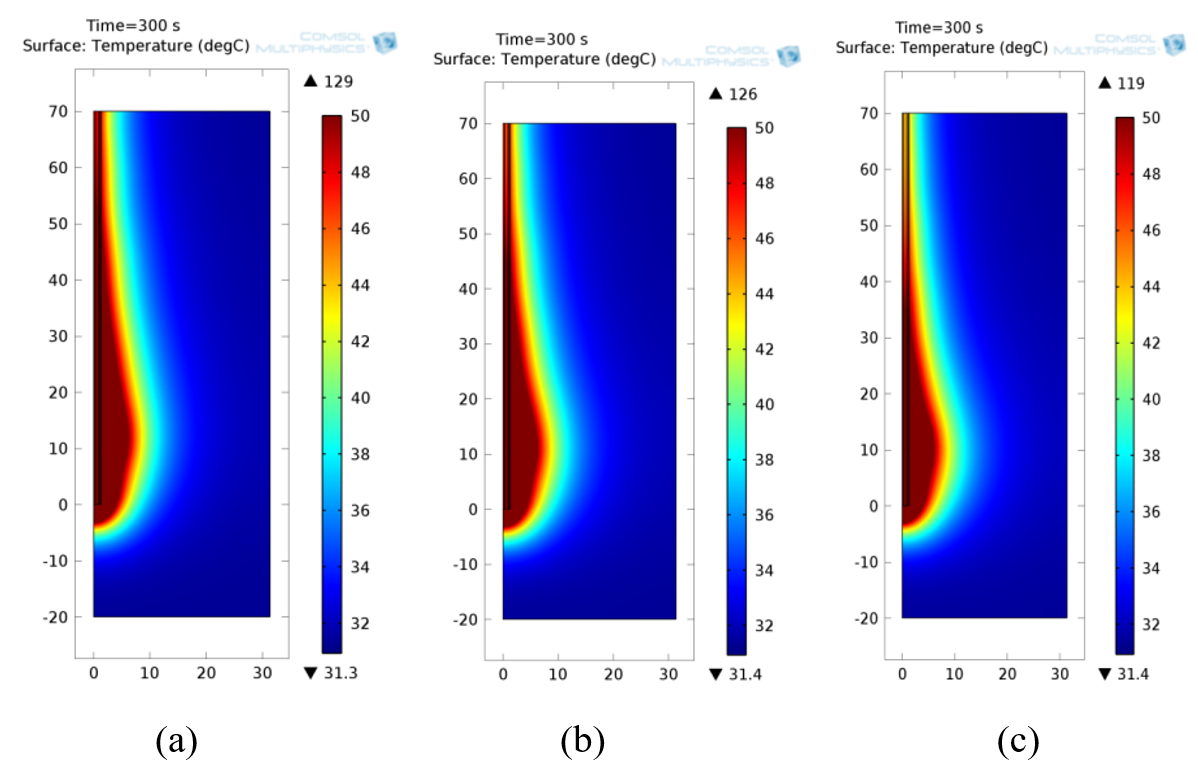
Figure 3: Temperature distributions using a monopole antenna with radiating length 10mm at a microwave power input of 10 W. The isotherm at 50 ºC is highlighted. (a) at 4.18GHz (b) at 4.76GHz (c) at 5.44GHz
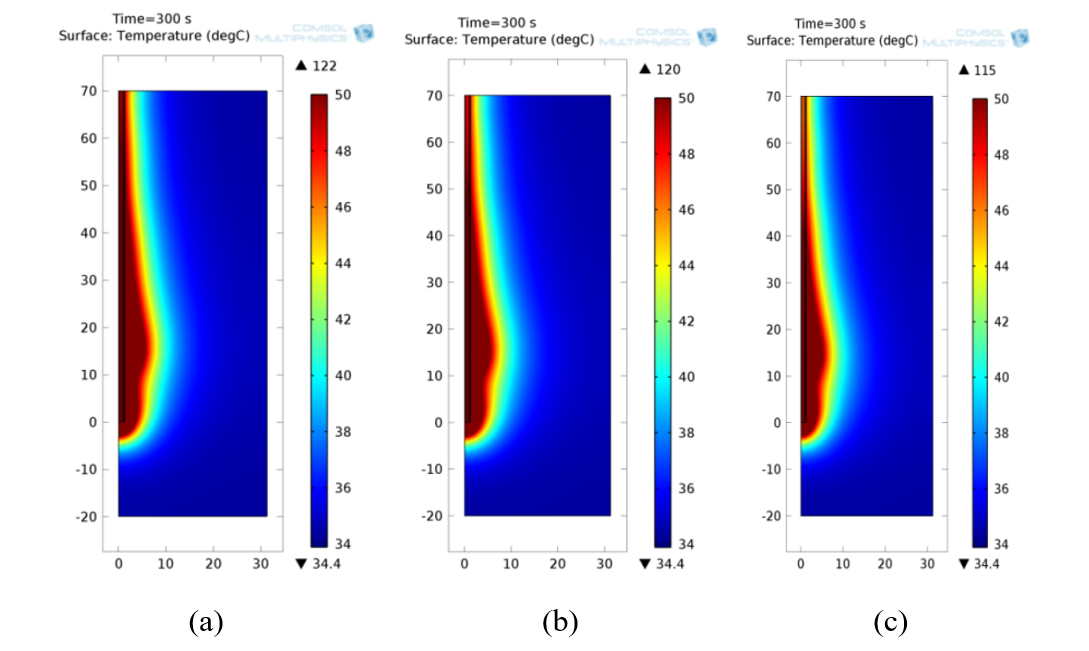
Figure 4: Temperature distributions using a monopole antenna with a radiating length of 13.5mm at a microwave power input of 10 W. The isotherm at 50 ºC is highlighted. (a) at 3.30GHz (b) at 3.56GHz (c) at 3.88G
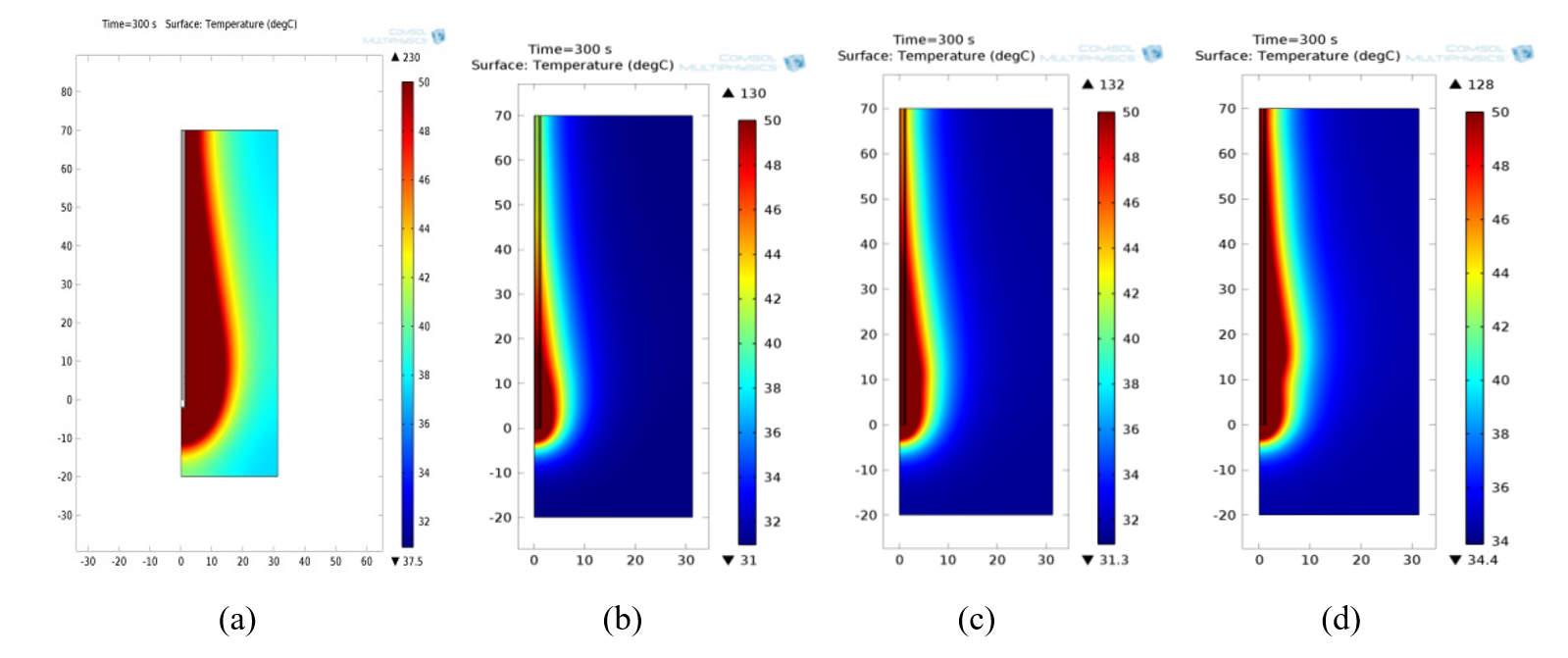
Figure 5: Temperature distributions for 2.45 GHz using (a) single slot antenna and monopole antenna with radiating length (b) 8 mm (c) 10 mm (d) 13.5 mm
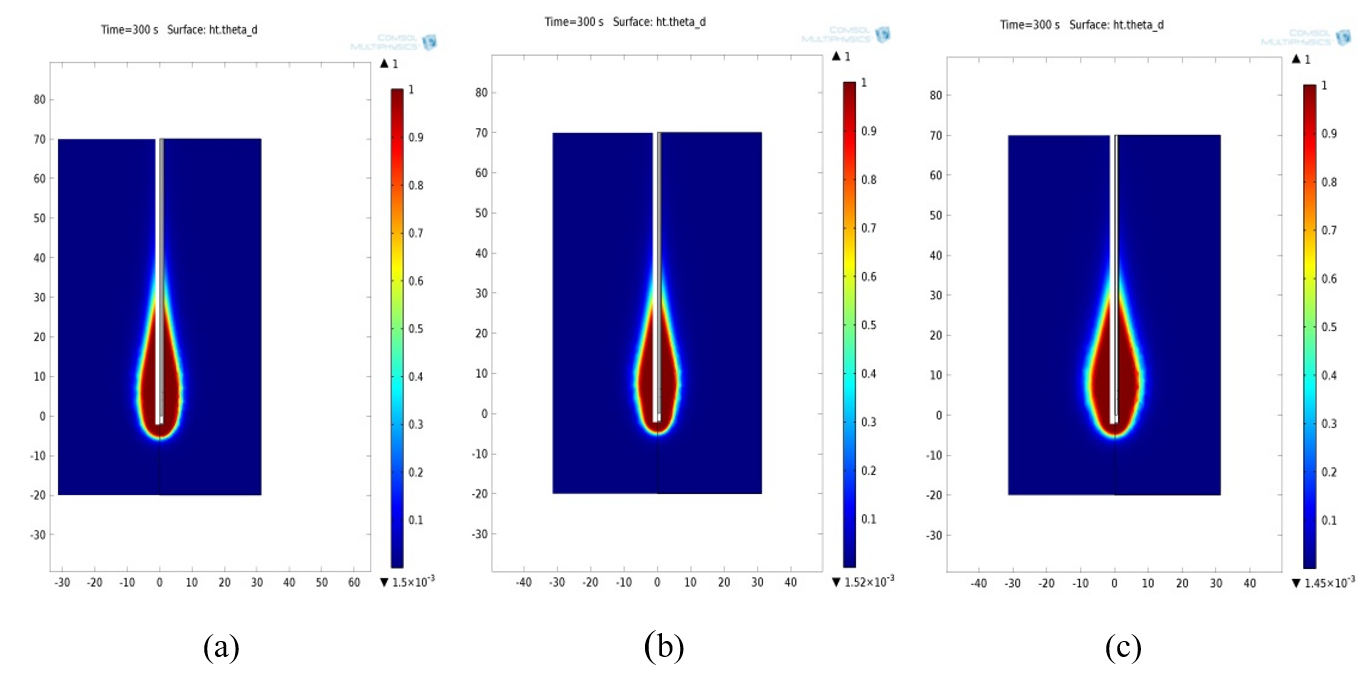
Figure 6: Necrotic tissue using single slot antenna at (a) 2.72GHz (b) 3.59GHz (c) 4.47 GHz
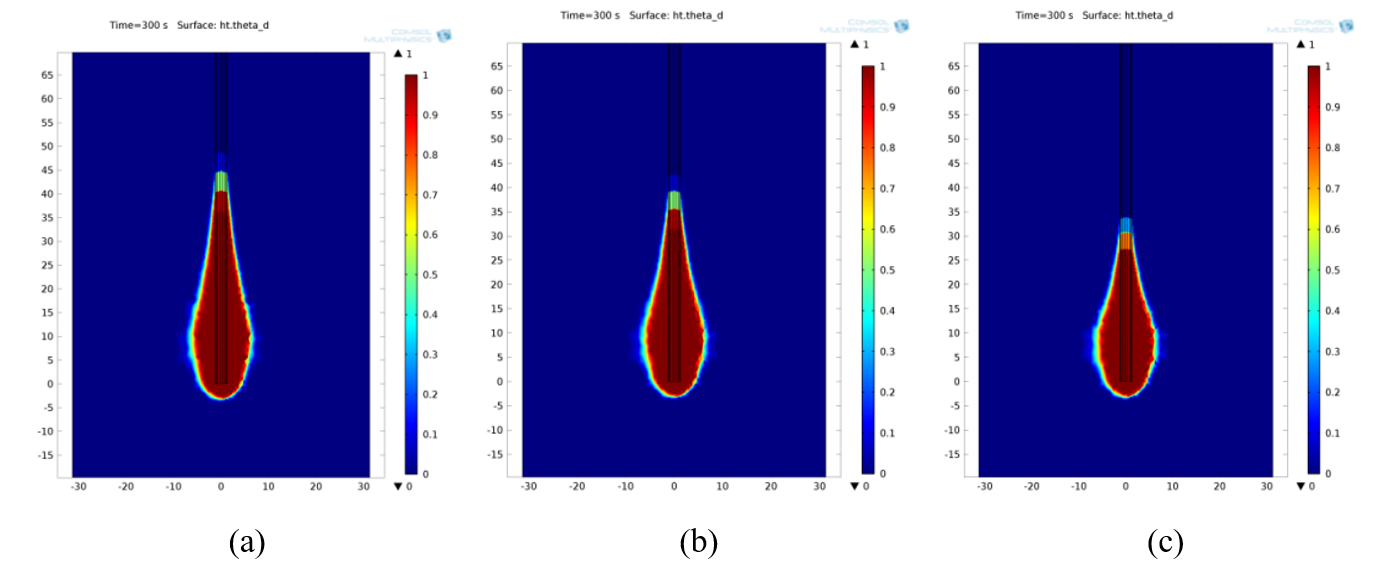
Figure 7: Necrotic tissue using monopole antenna with radiating length 8mm at (a) 5.44GHz (b) 6.02GHz (c) 6.61GHz
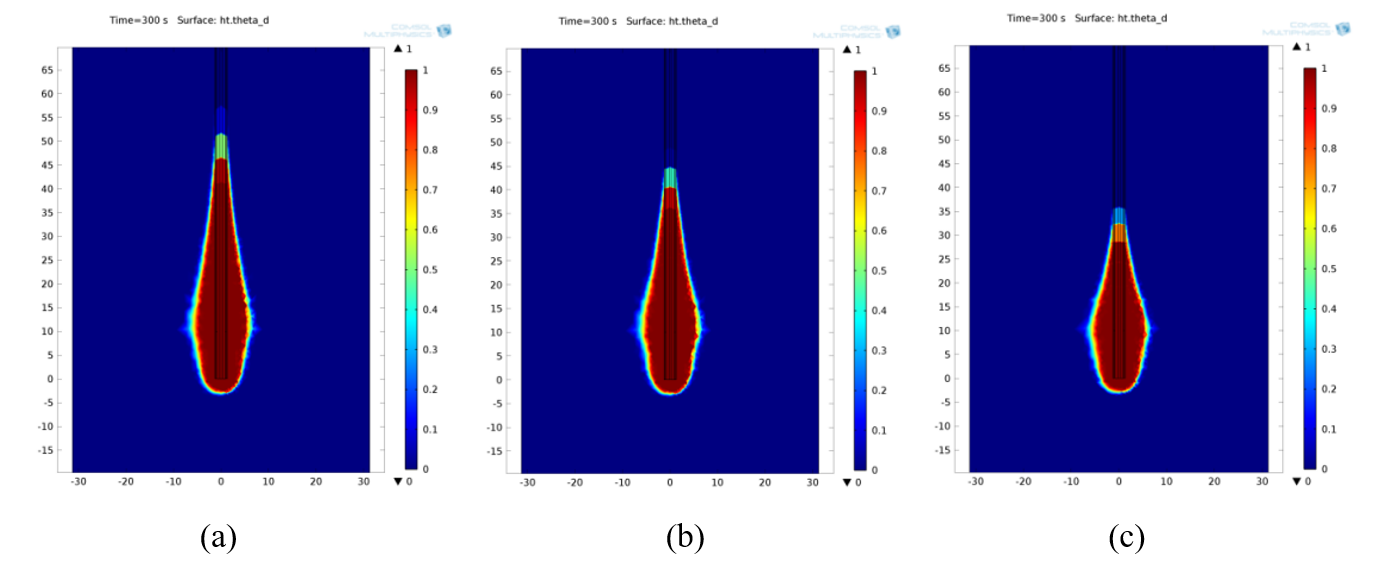
Figure 8: Necrotic tissue using monopole antenna with radiating length 10mm at (a) 4.18GHz (b) 4.76GHz (c) 5.44GHz
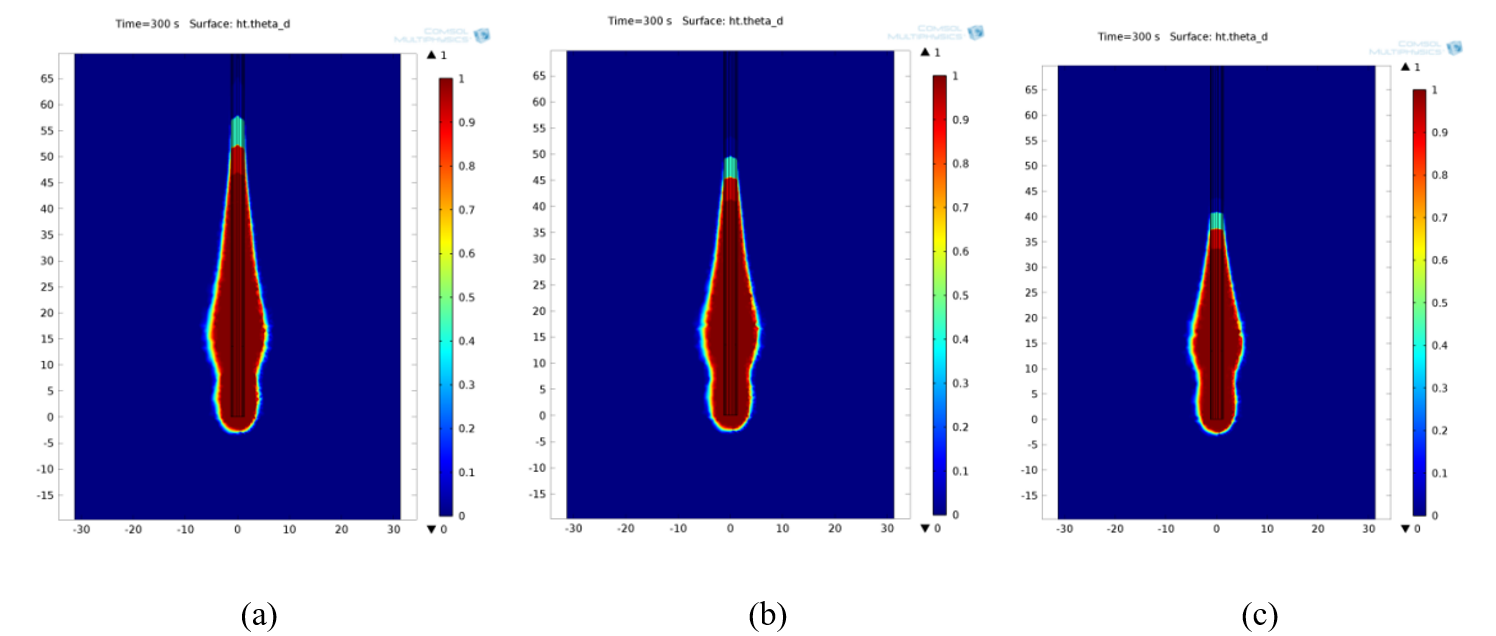
Figure 9: Necrotic tissue using monopole antenna with radiating length 13.5mm at (a) 3.30GHz (b) 3.59GHz (c) 3.88GHz
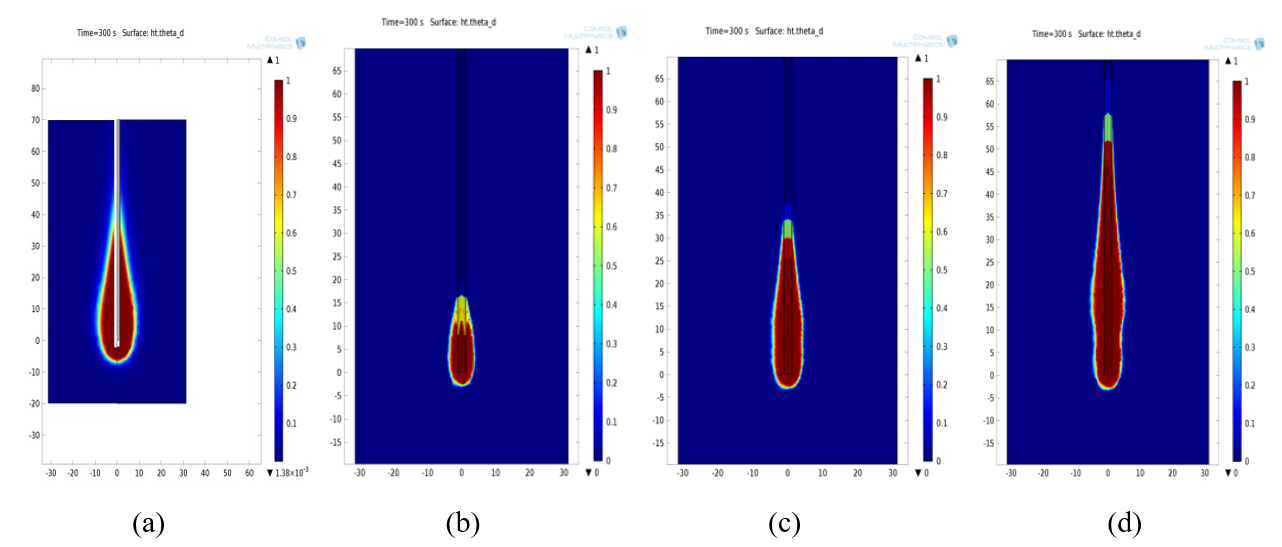
Figure 10: Necrotic tissue formed at 2.45 GHz using (a) single slot antenna and monopole antenna with radiating length (b) 8 mm (c) 10 mm (d) 13.5 mm
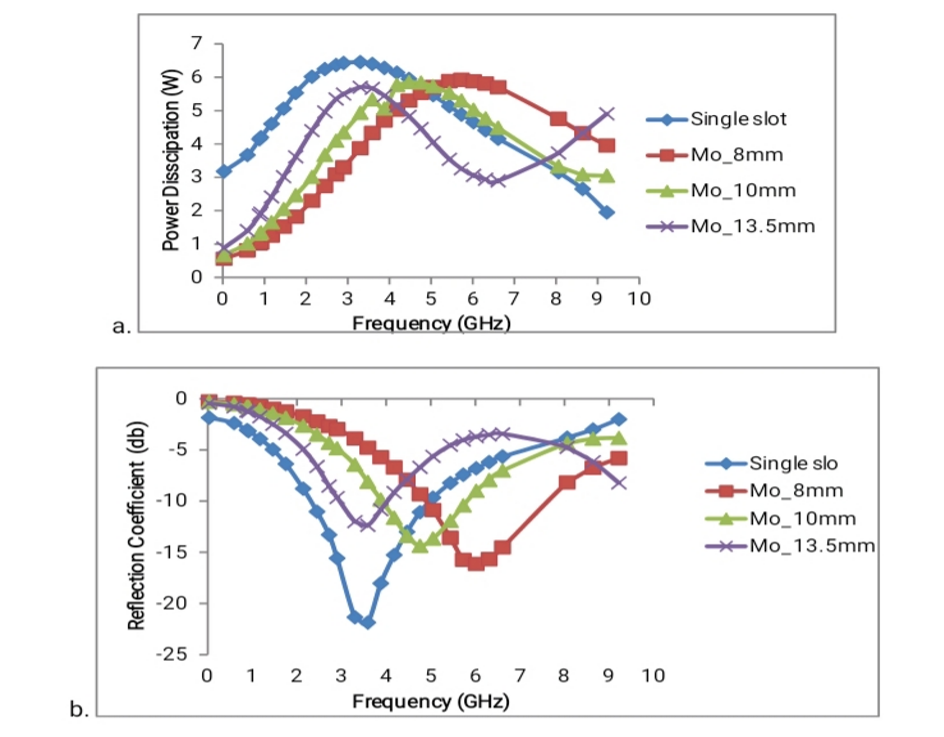
Figure 11: Comparison of power dissipations (a) and reflection coefficients (b) at variable frequencies with simulated microwave antennas
Figures 1-5 show the temperature distribution of breast tissue at a microwave power input of 10 W for the simulated antennas. The isotherm at 50 ºC was highlighted. The frequencies chosen from each antenna were based on power dissipation and reflection coefficient. The result of the temperature distribution from the simulated microwave antennas operating at their selected frequencies, a single slot antenna distributed at a higher temperature with the selected frequencies compared to all other antennas (Figure 1). [16] Monopole antenna with radiating length of 8 mm gave a much better distribution at 6.02 GHz and 6.61 GHz frequencies respectively (Figure 2b and Figure 2c), followed by a monopole antenna with radiating length of 10mm at 5.44 GHz (Figure 3c). The frequently used 2.45 GHz is distributed at a much higher temperature, irrespective of the antenna type (Figure 5).
Figures 6-10 show necrotic breast tissue at a microwave power input of 10 W at 50 using the simulated antennas. The heating patterns were ellipsoidal or tear-drop-shaped. This is because of the antenna geometry [17] From the selected frequencies using the single slot antenna, 4.47 GHz gave a better heating pattern compared to other frequencies (Figure 6c). Using the monopole antenna with a radiating length of 8 mm, frequencies 6.02 GHz and 6.61 GHz (Figure 7b and Figure 7c) gave a better heating pattern (ellipsoidal). Monopole antenna with a radiating length of 10 mm gave a better heating pattern (ellipsoidal) at 5.44 GHz (Figure 8c). No better heating pattern was produced by the monopole antenna with a radiating length of 13.5 mm; the heating pattern (ellipsoidal) grows closely along the antenna (Figure 9). In Figure 10, the single slot antenna gave a better heating pattern compared to other simulated antennas.
From Figure 11a, the Single slot antenna was found to have the highest power dissipation of 6.46 W at 3.30 GHz and minimum dissipation of 1.95 W at 9.22 GHz. Power dissipated by the monopole antennas was affected by their radiating lengths. The monopole antenna with a radiating length of 8 mm has the lowest power dissipation of all three monopole antennas: 0.56 W at 0.03 GHz, having the highest dissipation of 5.93 W at 5.73 GHz. The frequency used, 2.45 GHz, for tissue ablation gave a high-power dissipation of 6.25 W using the single slot antenna and a lower dissipation using monopole antennas. The monopole antennas gave a better power dissipation than the single slot antenna, irrespective of the frequencies [18]
The reflection coefficient is necessary to measure the efficiency of the microwave antenna used [18] From Figure 11b, the Single slot has the lowest reflection coefficient compared to all other antennas, -21.88 dB at 3.59 GHz, and the highest reflection coefficient of -1.86 dB at 0.03 GHz. Monopole antenna with a radiating length of 8 mm has the highest reflection coefficient compared to all other antennas, having a value of -0.27 dB at 0.03 GHz, and the lowest reflection coefficient of -16.14 dB at 6.02 GHz.
From the simulated result, it was found that frequency affects the way each antenna transfers power to the tissue. The single slot antenna proves best in transferring power more efficiently to the breast tissue. Antennas operating with high reflection coefficients and power dissipation can cause overheating of the feedline, possibly leading to damage to the coaxial line and the surrounding healthy tissues. Table 3 shows the ablation zone dimensions of breast tissue at a microwave power input of 10 W at 50 using the simulated antennas.
| Ablation zone dimensions of a simulated single slot antenna | ||||
| Frequency (GHz) | 2.45 | 2.72 | 3.59 | 4.47 |
| Diameter (mm) | 16.58 | 12.46 | 12.30 | 14.92 |
| Length (mm) | 41.58 | 38.06 | 36.61 | 38.87 |
| Aspect ratio | 0.34 | 0.33 | 0.42 | 0.42 |
| Ablation zone dimensions of a simulated monopole antenna with a radiating length 8 mm | ||||
| Frequency (GHz) | 2.45 | 5.44 | 6.02 | 6.61 |
| Diameter (mm) | 6.83 | 11.64 | 11.64 | 11.15 |
| Length (mm) | 13.16 | 46.90 | 40.86 | 32.41 |
| Aspect ratio | 0.61 | 0.25 | 0.28 | 0.37 |
| Ablation zone dimensions of a simulated monopole antenna with a radiating length 10 mm | ||||
| Frequency (GHz) | 2.45 | 4.18 | 4.76 | 5.44 |
| Diameter (mm) | 7.64 | 10.16 | 10.32 | 10.33 |
| Length (mm) | 32.35 | 47.50 | 43.23 | 31.61 |
| Aspect ratio | 0.27 | 0.22 | 0.25 | 0.32 |
| Ablation zone dimensions of the simulated monopole antenna with radiating length 13.5 mm | ||||
| Frequency (GHz) | 2.45 | 3.30 | 3.59 | 5.44 |
| Diameter (mm) | 8.94 | 10.33 | 9.67 | 9.05 |
| Length (mm) | 54.51 | 52.32 | 48.39 | 40.65 |
| Aspect ratio | 0.18 | 0.19 | 0.20 | 0.22 |
Table 3: Ablation zone dimensions of breast tissue
Frequency 2.45 GHz was imputed on the table for comparison, as it is mostly used for microwave ablation. The goal of MWA is to elevate the temperature in the unwanted tissue to 50°C and above, where cancer cells are destroyed [19,20] From this study, it was discovered that antenna geometry affects the dimension (size) of the necrotic tissue (ablated zone). Simulated single slot antenna gave the largest dimension of necrotic tissue compared to all other simulated antennas used in this study. From the selected frequencies using the single slot antenna, frequency 2.45 GHz gave the largest diameter of 16.58 mm with an aspect ratio of 0.34, followed by 4.47 GHz, having a diameter of 14.92 mm with an aspect ratio of 0.42.
Results from the simulated monopole antennas show that the monopole antenna with a radiating length of 8 mm gave the largest diameter compared to all other monopole antennas. The largest diameter from this antenna was 11.64 mm at frequencies 5.44 and 6.02 GHz, respectively, having an aspect ratio of 0.25 for 5.44 GHz and 0.28 for 6.02 GHz. The least dimension was found with 2.45 GHz, having a diameter of 6.83 mm with an aspect ratio of 0.61.
Monopole antenna with a radiating length of 10 mm gave the largest diameter of 10.33 mm at 5.44 GHz, having an aspect ratio of 0.32 compared to all other selected frequencies using the same antenna. Monopole antenna with a radiating length of 13.5 mm gave the highest necrotic length compared to all other antennas. Its largest diameter was 10.33 mm at 3.30 GHz. Again, 2.45 GHz has the lowest dimension, but its length, 54.51 mm, was higher compared to other frequencies. So far, it was found that the frequency with the least dimension, irrespective of the simulated antenna type, has the highest aspect ratio. This was due to the increased length of the necrotic (ablated zone) breast tissue. As the length of the necrotic breast tissue increases, the diameter decreases with increased aspect ratio.
In comparison with a related study using a single slot coaxial antenna operating at 2.45 GHz, showed that the reflection coefficient in normal adipose-dominated tissue was -2.82 dB, the maximum temperature distribution was 116.03 ºC, and the ablation zone radius was 53 mm using an isotherm at 60 ºC.[12] While in breast cancer tissue, the reflection coefficient calculated for the frequency at 2.45 GHz was -6.38 dB (which is higher compared to the simulated result i.e. -11.03dB), the maximum temperature distribution was 125.96 ºC (which is lower compared to the result from the simulation using the same antenna and frequency having a maximum temperature of 128, though with an isotherm of 50 ), and the ablation zone radius was 92 mm. From the comparison, differences in the simulated results from both studies could be influenced by the antenna geometry. Using an open-tip antenna with radiating length 20 mm operating with a microwave power of 50 W at 2.45 GHz and an ablation time of 180 s, results showed a maximum temperature of 150. Although a high power (50 W) and a much shorter time of 180 s were used, the temperature distribution is higher compared to the simulated result using the open-tip monopole antennas, irrespective of their radiating length [9] Thus, antenna geometry, microwave power, and time influence the outcome of the simulated results.
Low frequencies selected for this study were intended to give a better heating depth of penetration; higher frequencies would give less. Study from experienced a heating depth which was only a few millimeters inside the cancer using a planar coaxial microwave antenna at a higher frequency of 18 GHz and a low power input of 1 W for 5 min on nude mice xenografted with human breast cancer [21] The core temperature of ex vivo cancer after 5-min ablation was 64 and for an in vivo study while the surface temperature of the antenna reached. This means that the heat source generation is limited to within a few millimeters of the applicator. The heating depth can be increased by increasing the power level, which will enhance thermal conduction through the target.
Conclusion
The data from this study indicates that frequency impacts how antennas transfer power to tissue. The temperature distributions of different antenna types operating at a low power dissipation and reflection coefficient were examined. Power dissipation for all simulated microwave antennas was above 50% from an input power of 10 W. Simulated single slot antenna proved to be efficient, but with a high power dissipation of 59.5%. Simulated monopole antenna with radiating length 8 mm proves to be outstanding compared to all other simulated monopole antennas. The frequency of 6.02 GHz has the lowest reflection coefficient of -16.14 dB, but has a high-power dissipation of approximately 59%. Compromising between power dissipation, backward heating along the antenna shaft, and aspect ratio of necrotic tissue, a simulated monopole antenna with radiating length 8 mm operating at 6.61 GHz is more efficient, having a power dissipation of 57%.
References
- World Health Organization. Breast cancer. 2010 Breast cancer
- Rubio MFJC, Hernández AV, Salas LL. High temperature hyperthermia in breast cancer treatment. J Cancer Res Ther. 2013;9(2):219-225 Crossref | Google Scholar
- Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics: GLOBOCAN estimates incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209-249 PubMed | Crossref | Google Scholar
- Simon JC, Dupuy DE, Mayo-Smith WW. Microwave ablation: principles and applications. Radiographics. 2005;25(1):69-83 PubMed | Crossref | Google Scholar
- National Cancer Institute Microwave therapy. 2010 Microwave therapy
- Acikgoz H, Mittra R. Microwave coaxial antenna for cancer treatment: reducing the backward heating using a double choke. In: Proceedings of the 2015 International Symposium on Antennas and Propagation (ISAP). IEEE; 2015:1-4 Google Scholar
- Aykut E, Zeynep A, Oğuz T, Burak T. Numerical analysis of microwave cancer therapy using single and double slot antennas for breast and liver tissues. J Ther Sci Tech. 2022;42(1):37-48 Crossref | Google Scholar
- Hand JW. Modeling the interaction of electromagnetic fields (10 MHz-10 GHz) with the human body: methods and applications. Phys Med Biol. 2008;53:243-286 PubMed | Crossref | Google Scholar
- Sanpanich A, Phasukkit P, Sueaseenak D, Kajornpreedanon Y, Hamamoto K, Pintavirooj C. A basic investigation of cancerous breast microwave ablation using opened-tip applicator and ex vivo experiment. J Vasc Interv Radiol. 2017;28(5):723-730 A basic investigation of cancerous breast microwave ablation using opened-tip applicator and ex vivo experiment
- Tungjitkusolmun S, Staelin ST, Haemmerich D, Tsai JZ, Cao H, Webster JG, Lee FT, Mahvi DM, Vorperian VR. Three-dimensional finite-element analyses for radio-frequency hepatic tumor ablation. IEEE Trans Biomed Eng. 2002;49(1):3-9 PubMed | Crossref | Google Scholar
- Saito K, Hayashi Y, Yoshimura H, Ito K. Heating characteristics of array applicator composed of two coaxial-slot antennas for microwave coagulation therapy. IEEE Trans Microwave Theory Tech. 2000;48(11):1800-1806 Crossref | Google Scholar
- Cepeda Rubio MFJ, Vera Hernández A, Leija Salas L. High temperature hyperthermia in breast cancer treatment. In: Huilgol N, ed. Hyperthermia. Rijeka, Croatia: IntechOpen; 2013 Crossref | Google Scholar
- Deshan Y. Measurements, antenna design and advanced computer modeling for microwave tissue ablation. 2006. Retrieved from Measurements, antenna design and advanced computer modeling for microwave tissue ablation | Guide books (acm.org) Google Scholar
- IFAC Italian National Research Council. Calculation of the dielectric properties of body tissues (breast fat) in the frequency range 10 Hz – 100 GHz. 1997-2012. Institute for Applied Physics. 2012 Dielectric Properties of Body Tissues
- Brace CL. Microwave tissue ablation: biophysics, technology and applications. Crit Rev Biomed Eng, 2010;38(1):65-78 PubMed | Crossref | Google Scholar
- Marwa S, Amjad I, Amor S, Mohamed I.W, Hafedh B. (2022). Modeling of heat transfer distribution in tumor breast cancer during microwave ablation therapy. Microwave and optical technology letters. 2022;64(8):1364-1375 Crossref | Google Scholar
- Brace CL. Microwave ablation technology: what every user should know. Curr Probl Diagn Radiol. 2009;38(2):61-67 PubMed | Crossref | Google Scholar
- Gas P. The S11 parameter analysis of multi-slot antenna with periodic slots. In: Analysis and Simulation of Electrical and Computer Systems. 2018:367-376 Crossref | Google Scholar
- Pisa S, Cavagnaro M, Bernardi P, Lin JC. A 915-MHz antenna for microwave thermal ablation treatment: physical design, computer modeling and experimental measurement. IEEE Trans Biomed Eng. 2001;48(5):599-601 PubMed | Crossref | Google Scholar
- Marwa S, Abdullah B, Hafedh B. Effects of target temperature on thermal damage during temperature-controlled MWA of liver tumor. Case Stud Therm Eng. 2022;31:101821 Crossref | Google Scholar
- Yoon J, Cho J, Kim N, Kim D, Lee E, Cheon C, et al. High-frequency microwave ablation method for enhanced cancer treatment with minimized collateral damage. Int J Cancer. 2010;129(8):1970-1978 PubMed | Crossref | Google Scholar
Acknowledgments
Not reported
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author Information
Corresponding Author:
Amiegbereta Edwin Ehis
Department of Physics
Dennis Osadebay University, Asaba, Delta State, Nigeria
Email: edwin.amiegbereta@dou.edu.ng
Co-Authors:
Esi Oghenevovwero Emmanue
Department of Physics
Dennis Osadebay University, Asaba, Delta State, Nigeria
Ibitoye Ayo Zacchaeus
Department of Radiation Biology
Radiodiagnosis and Radiotherapy, University of Lagos, Lagos, Nigeria
Authors Contributions
All authors contributed to the conceptualization, investigation, and data curation by acquiring and critically reviewing the selected articles. They were collectively involved in the writing – original draft preparation, and writing – review & editing to refine the manuscript. Additionally, all authors participated in the supervision of the work, ensuring accuracy and completeness. The final manuscript was approved by all named authors for submission to the journal.
Ethical Approval
Not reported
Conflict of Interest Statement
The authors declare no conflicts of interest.
Guarantor
None
DOI
Cite this Article
Amiegbereta EE, Ibitoye AZ, Esi OE. Computational Analysis of a Suitable Antenna and Optimized Frequency for Microwave Ablation of Breast Cancerous Tissue. medtigo J Med. 2024;2(3):e13752246. doi:10.63096/medtigo3062249 Crossref









