Author Affiliations
Abstract
Acute Aortic Occlusion (AAO) is an infrequent but severe vascular emergency with a high mortality rate, necessitating prompt recognition and intervention. This article highlights a case study to enhance awareness among emergency physicians regarding the early signs of AAO. A 56-year-old man with a history of hypertension and COPD presented to the emergency department (ED) with cramps in both legs that persisted for three hours. Initially, his examination was normal, but his pain worsened despite medication. Suspecting abdominal aortic occlusion, the clinical team monitored the patient closely. Within seven hours, his legs became numb, paralyzed, cold, mottled, and lacked a pulse. A CT aortogram revealed atherosclerotic disease with a thrombus in the thoraco-abdominal aorta. The patient was transferred to a specialized facility for surgery, but his condition rapidly deteriorated, leading to his death shortly after. The case underscores the rarity of AAO, with an incidence of 3.8 per million person-years, and the necessity for a high amount of suspicion. Key indicators included intractable leg pain and progressive ischemic symptoms. The patient’s age, gender, and comorbidities prompted clinical suspicion before imaging. The article stresses the critical role of thorough history taking, physical examination, continuous monitoring, and re-evaluation in the ED. In conclusion, despite AAO’s rarity, this case illustrates the importance of considering it in patients presenting with leg pain and risk factors for vascular disease. Clinicians should maintain a high level of suspicion and act swiftly to improve patient outcomes.
Keywords
Acute Aortic Occlusion (AAO), Aortoiliac Occlusive Disease (AIOD), Vascular emergency, Emergency medicine, Aneurysmal dilatation, Tramadol, Lumbar osteophytosis
Introduction
Acute Aortic Occlusion is infrequent but life-threatening vascular emergency with an incidence of 3.8 per 1-million-person years [1]. This has a high degree of morbidity and with 30-day mortality of about 20%-70% [2]. Dyslipidemia, male gender, smoking, diabetes mellitus and hypertension are the main risk factors. The most common causes of aortic obstructions are large saddle thromboembolism to the aortic bifurcation, in situ thrombosis of an atherosclerotic aorta and occlusion of previous surgical reconstructions [3]. Clinical features include lower limb pain, sensory deficit, weakness and paralysis [4]. Aortic occlusion requires early recognition and intervention for revascularization. Hence, this is an important condition that needs to be recognized by the physicians responsible for the assessment of the patient. The purpose of this case report is to describe a case of acute aortic disease, identify clinical characteristics that raise a high suspicion of the disease, and talk about the diagnostic strategy used in this instance.
Case Presentation
A 56-year-old male presented to the emergency department with the sudden onset of leg pain that started seven hours ago. He was a known case of hypertension as well as COPD. He also had a 21-pack-year social history of smoking. The patient experienced sudden excruciating pain in the bilateral lower extremity, crampy in character, 8/10 in severity, with no noted discoloration, but cold to the touch. Pain started on the left leg, then progressed to the right lower leg. These symptoms were associated with abdominal pain, 5/10 in severity, in the epigastric area, but non-radiating to the back, lasting for a few minutes, relieved by passage of flatus. The lower extremities were cold, “marble white” skin, pale, weak pulse dorsalis pedis. Motor 4/5 with 100 % sensory, computed ABI was 0.86. Other physical findings were within normal limits at the time of examination.
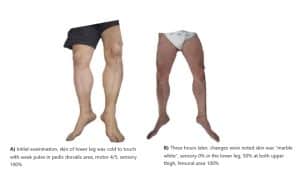
Figure 1: Difference in the patient’s leg appearance from the time the patient sought consultation
Case Management
The patient was initially given paracetamol 1 gram, then tramadol 50 mg TIV, eventually nalbuphine 2 mg TIV because of intractable pain. At that time, the emergency physician was considering myositis vs. vascular occlusion. Routine labs were done. ECG revealed sinus rhythm, T wave inversion at V5-6, AVL, and lead 1. CBC showed leukocytosis with neutrophilic predominance. Chest x-ray revealed progression in the degree of mild pulmonary congestive changes as well as suspicion of concomitant pneumonia in the right lower lobe. Lumbosacral x-ray revealed a decompression deformity T 11. FPA supine and upright results were segmental adynamic ileus, which prompted consideration of hepatomegaly and lumbar osteophytosis. Hence, the patient was referred to Vascular (IM service) and TCVS for further evaluation and management. A Stat AV duplex scan was advised but not available in the ED. Hence abdominal CT scan (Figure 2 and Figure 3) with contrast and CT aortogram was performed. Tomography revealed atherosclerotic thoraco-abdominal aorta with mural thrombus formation, aneurysmal dilatation at the level of the ascending aorta, transverse arch, celiac artery, superior mesenteric artery, and renal artery, no dissection or contrast extravasation. Thus, the patient was then administered a heparin drip 10, 000 units in 100 cc to run for 10 cc/hr (18 units/kg/hr). Cefepime 2 g TIV as a loading dose for pneumonia was given as well.

Figure 2: Abdominal CT scan (axial view) showing extensive aortic occlusion
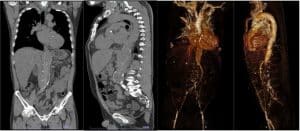
Figure 3: Abdominal CT scan and CT aortogram (coronal and sagittal view)
The patient’s medical condition was accurately assessed, and he was transferred to the Philippine Heart Center for definitive management. But the patient’s condition worsened, ultimately resulting in his death.
Discussion
In the case presented, it is very important to have a high clinical suspicion in patients with severe intractable leg pain for a vascular disease. The medical history of hypertension, dyslipidemia, and a long history of smoking were essential risk factors in this case. Vascular evaluation through physical examination is essential to be performed in this case. Hence, inspection of skin for any signs of ischemia, such as pale or “marble skin”, cyanotic nail beds, was appreciated. Thus, a weak pulse or absence of pulse in the femoral, popliteal, or dorsal pedis would raise concern to measure the ankle-brachial index. The computed ABI 0.86 suggests that the patient has moderate arterial disease, and a vascular specialty is warranted.
Imaging is an important tool in determining the location of the possible obstruction. In this case, thromboembolism was located at thoraco-abdominal aorta which led to an aneurysmal dilatation at the level of the ascending aorta, transverse arch, celiac artery, superior mesenteric and renal artery. These signs manifest as an abdominal pain in the patient.
We have seen that the lower leg’s motor and sensory functions alter with time, even with the obstruction in the large vessel. This could be because the lower extremities are still supplied by collateral arteries.
The case required a multidisciplinary approach. This involved the Internal medicine – vascular service and General Surgery- TCVS in providing definitive management for the patient. The patient was sent to a specialty hospital with the explicit purpose of undergoing surgical thrombo-embolectomy and revascularization. However, the patient’s condition steadily declined, ultimately resulting in his death.
It is worth to note that the research shows that the survival rate of patients with aortoiliac occlusive disease is influenced by the surgical success, long-term permeability of the graft, management of risk factors, and the cessation of tobacco use, which is unfavorable in this case [5].
It is important to conduct a thorough medical history and extensive physical examination of patients experiencing sudden and unmanageable leg pain. Persistent pain should prompt immediate referral to a specialist and consideration for admission for monitoring and further assessment. Misdiagnosis with conditions like peripheral neuropathy, musculoskeletal strain, lumbar spine compression, or myositis is possible. This case highlights the significance of medical history and vascular examination in the emergency department. To prevent misdiagnosis, it is crucial to carefully examine patients with unmanageable leg pain and consider vascular occlusive disease.
Conclusion
The presented case of a 56-year-old male with AIOD underscores the critical importance of prompt diagnosis and intervention in vascular emergencies. Acute Aortic Occlusion, though rare, carries a significant risk of morbidity and mortality, particularly if recognition and treatment are delayed. This case highlights the need for a high index of suspicion when patients present with a sudden onset, intractable leg pain, especially in the presence of risk factors such as hypertension and smoking. Effective management requires a multidisciplinary approach, including timely imaging, vascular assessment, and surgical intervention. Despite appropriate measures, the outcome in this case was unfavorable, emphasizing the aggressive nature of AIOD and the challenges it presents in emergency care. Awareness of this condition, coupled with early intervention, is essential for improving patient outcomes in similar cases.
References
- Grip O, Wanhainen A, Björck M. Acute aortic occlusion. 2019;139(2):292-294. PubMed | Crossref | Google Scholar
- Mohapatra A, Salem KM, Jaman E, Robinson D, Avgerinos ED, Makaroun MS, Eslami MH. Risk factors for perioperative mortality after revascularization for acute aortic occlusion. J Vasc Surg. PubMed | Crossref | Google Scholar
- Brown KN, Muco E, Gonzalez L. Leriche syndrome. StatPearls. PubMed
- Robinson WP, Patel RK, Columbo JA, et al. Contemporary management of acute aortic occlusion has evolved but outcomes have not significantly improved. Ann Vasc Surg. 2016;34:178-186. PubMed | Crossref | Google Scholar
- Indes JE, Mandawat A, Tuggle CT, et al. Endovascular procedures for aorto-iliac occlusive disease are associated with superior short-term clinical and economic outcomes compared with open surgery in the inpatient population. J Vasc Surg. 2010;52(6):1173-1179. PubMed | Crossref | Google Scholar
Acknowledgments
Not reported
Funding
Not reported
Author Information
Corresponding Author:
John Emmanuel D. Velasco
Department of Emergency Medicine
Veterans Memorial Medical Center Quezon City, Philippines
Email: dalcoje@gmail.com
Co-Author:
Janina Bianca Ortiz
Department of Emergency Medicine
Veterans Memorial Medical Center Quezon City, Philippines
Authors Contributions
All authors contributed to the conceptualization, investigation, and data curation by acquiring and critically reviewing the selected articles. They were collectively involved in the writing – original draft preparation and writing – review & editing to refine the manuscript. Additionally, all authors participated in the Supervision of the work, ensuring accuracy and completeness. The final manuscript was approved by all named authors for submission to the journal.
Informed Consent
Patient consent has been taken.
Conflict of Interest Statement
None
Guarantor
Not reported
DOI
Cite this Article
Velasco JE, Bianca Ortiz J. Aortoiliac Occlusive Disease. medtigo J Med. 2024;2(3):e3062244. doi:10.63096/medtigo3062244 Crossref









