Author Affiliations
Abstract
Childhood cancers are a leading cause of death by disease beyond infancy. In developed countries, leukemia is the most common, followed by brain tumors and lymphomas, while in developing regions, lymphomas and nephroblastoma are more prevalent. This study investigates the patterns in the Kurdistan Region of Iraq. The study aims to identify the five most common cancers in children under 10 in Kurdistan and analyze their incidence to encourage further research and support for affected children. This cross-sectional study used data from Erbil’s cancer registry, covering pediatric cases from January 2015 to January 2019. The data, analyzed by age group and cancer type, were accessed with ethical approval from local health authorities. Among 374 cases, leukemia was the most common cancer (32%), followed by complex mixed and stromal neoplasm (13%), lymphoma (13%), neuroepitheliomatous neoplasm (11%), and glioma (7%). There were 210 male and 163 female cases. The study offers insight into childhood cancers in Kurdistan, highlighting areas for further research and resource allocation.
Keywords
Cancer, Kurdistan, Erbil, Leukemia, Children, Neoplasm, Tumors, Morphology, Topography.
Introduction
Along with the major advancements that medicine has experienced in the last few decades, there undoubtedly has been an increase in efforts and attention put into improving the quality of life within the pediatric age group. With that being said, it’s important to analyze the incidence pattern of pediatric malignancies so that further actions can be made to improve pediatric cancer care locally as well as globally. As reported by the American National Institutes of Health (NIH), even though malignancies are rare in children, they remain the leading cause of death by disease past infancy among children in the United States (U.S). In fact, it is estimated that in 2021, 15,590 children and adolescents ages 0 to 19 in the U.S. will be diagnosed with cancer, and 1,190 will die of the disease [1]. By identifying the most common cancers, the extent of one of the biggest threats to children in our region will be pointed out. This provides numerous benefits, facilitates further research in the field, guides allocation of resources where they are needed the most, sheds light on the variations between our results and international data, and enables us to track changes in incidence over time. Through a literature review, it was observed that the most common histological types of childhood malignancies reported globally were (in decreasing order of incidence): leukemias, brain malignancies, lymphomas, and solid tumors (such as neuroblastoma and Wilms tumors) [2].
Unlike the developed countries, the most common histologic types of pediatric tumors in Africa were reported to be lymphomas, nephroblastoma, Kaposi sarcoma, and retinoblastoma after data were analyzed from 18 Sub-Saharan countries [3]. This finding indicates that the incidence of different types of pediatric cancers may vary across the world, and this in turn creates a need for research to be conducted in the Kurdistan Region of Iraq. According to a study conducted in Sulaymaniyah province using data from 2006 to 2014, the most common malignancies by primary site were leukemia, lymphoma, brain, kidney, and bone [4]. No similar studies have been published in Erbil, Kurdistan. A critical problem in the fight against pediatric malignancies in Kurdistan, Iraq, as well as a good proportion of the rest of the developing countries, has been a lack of coordinated, wide-scale information gathering (data collection) in addition to an insufficiency of research. This will, in turn, hinder the management of pediatric cancer cases and, as a result, may heavily impact the quality of life in such patients as well as their life expectancy.
The goal of this study, therefore, is to have an insight into the incidence of cancer in the pediatric population within the Kurdistan Region of Iraq, and to determine the top 5 most common cancers. With such results, we aim to provide a step forward towards better analysis of the pattern of incidence in childhood malignancies in the region, a stimulus for further research on the etiology of childhood cancer, and a more targeted management plan, along with efficient distribution of funding and medical efforts towards childhood cancers.
Methodology
This is a cross-sectional descriptive epidemiological study, using secondary data obtained from Erbil’s cancer registry of pediatric patients from January 2015 to January 2019. Access to the data was granted with the assistance of the Kurdistan Ministry of Health’s Cancer Department, as well as the Awat Radiation Oncology Center. Unfortunately, registry data for the years 2020 and 2021 were not available due to technical issues. It is to be noted that the data acquired included the complete medical records of 639 pediatric patients from cities all over Iraq who were being treated in Erbil. The system used to categorize the cancers is the International Classification of Diseases for Oncology, third edition (ICD-03), first published by the World Health Organization (WHO) in the year 2000. From the available data, only pediatric cases below the age of 10 from the Kurdistan Region of Iraq (KRG) were included. Therefore, cases above the age of 10 and/or cases living in the rest of Iraq were excluded from the database. Ultimately, only 374 cases of the original 639 cases were included in the study. Data analysis was conducted using the Microsoft Excel 2010 computer program. The research article has been written following the American Psychological Association (APA) style. The privacy of patients was of critical importance throughout the conduct of this research. The data was received from the Kurdistan (MOH), and codes for each case were assigned according to their registration IDs, without the names of patients, to conserve their privacy. All patients’ personal information will remain confidential. In relation to this research article, the authors have no conflict of interest to disclose.
Results
There was a total of 374 cases fitting the required criteria for this study. Out of these, the cancers were listed according to morphological and topographical classifications. The frequencies of childhood cancers according to their morphology, shown in Table 1, revealed that together, the top 5 cancers account for over 75% of cancers in children. According to their topography, the most common cancers were in the hematopoietic and reticuloendothelial systems (32.9%), urinary tract (12.8%), lymph nodes (8.3%), brain (7.5%), and bones, joints, and articular cartilage (6.4%). These results are displayed in Table 2. Out of a total of 50 cases of complex mixed and stromal neoplasms, 37 were mesoblastic nephromas and nephroblastoma, 9 were hepatoblastomas, 3 were clear cell sarcomas of the kidney, and 1 case was embryonal sarcoma (Figure 1). Out of a total of 41 cases of Neuroepitheliomatous Neoplasms, 24 were neuroblastomas, 13 were retinoblastomas, 3 were ganglioneuromas, and 1 case was atypical teratoid/rhabdoid tumor (Figure 2). The ratio of male to female cases was 210:163 (Figure 3). Regarding the distribution of the cases among different cities in Kurdistan, 79% were from Erbil, 11% from Duhok, 6% from Kirkuk, 3% unlisted, and 1% from Al Sulaimanyia (Figure 4). The number of cancer cases diagnosed increased from 34 in 2015 to 47 in 2016, followed by a significant spike to 105 in 2017. However, the number of diagnosed cases drastically dropped to 11 in 2018, before rising again to 84 cases in 2019 (Figure 5).
| Morphology | Number of cases | Percentage |
| Leukemias | 119 | 31.8181% |
| Complex mixed and stromal neoplasms | 50 | 13.3689% |
| Hodgkin and non-Hodgkin lymphomas | 47 | 12.5668% |
| Neuroepitheliomatous neoplasms | 42 | 11.2299% |
| Gliomas | 25 | 6.6844% |
| Miscellaneous bone tumors | 16 | 4.278% |
| Myomatous neoplasms | 15 | 4.0106% |
| Squamous cell neoplasms | 12 | 3.2085% |
| Germ cell neoplasms | 12 | 3.2085% |
| Basal cell neoplasms | 6 | 1.6042% |
| Ductal and lobular neoplasms | 5 | 1.3368% |
| Osseous and chondromatous neoplasms | 5 | 1.3368% |
| Neoplasms of histiocytes and accessory lymphoid cells | 5 | 1.3368% |
| Transitional cell papillomas and carcinoma | 4 | 1.0695% |
| Adenomas and adenocarcinoma | 4 | 1.0695% |
| Neoplasms | 1 | 0.2673% |
| Mucoepidermoid neoplasms | 1 | 0.2673% |
| Cystic, mucinous, and serous neoplasms | 1 | 0.2673% |
| Mesonephromas | 1 | 0.2673% |
| Mast cell tumors | 1 | 0.2673% |
| Myelodysplastic syndromes | 1 | 0.2673% |
| Unknown | 1 | 0.2673% |
Table 1: Incidence of cancers according to their morphology (histology)
| Topography | Number of cases | Percentage |
| Hematopoietic and reticuloendothelial systems | 123 | 32.8877% |
| Urinary tract | 48 | 12.8342% |
| Lymph nodes | 31 | 8.2887% |
| Brain | 28 | 7.4866% |
| Bones, joints, and articular cartilage | 24 | 6.4171% |
| Eye and adnexa | 18 | 4.8128% |
| Adrenal gland | 17 | 4.5454% |
| Connective, subcutaneous, and other soft tissues | 13 | 3.4759% |
| Liver | 12 | 3.2085% |
| Skin | 11 | 2.9411% |
| Other and ill-defined sites | 9 | 2.4064% |
| Testis | 7 | 1.8716% |
| Unknown primary site | 7 | 1.8716% |
| Peripheral nerves and the autonomic nervous system | 4 | 1.0695% |
| Breast | 4 | 1.0695% |
| Thyroid gland | 4 | 1.0695% |
| Stomach | 2 | 0.5347% |
| Ovary | 2 | 0.5347% |
| Spinal cord | 2 | 0.5347% |
| Border of the tongue | 1 | 0.2673% |
| Parotid gland | 1 | 0.2673% |
| Tonsil | 1 | 0.2673% |
| Nasal cavity and middle ear | 1 | 0.2673% |
| Accessory sinuses | 1 | 0.2673% |
| Bronchus and lung | 1 | 0.2673% |
| Heart, mediastinum, and pleura | 1 | 0.2673% |
| Vagina | 1 | 0.2673% |
Table 2: Incidence of cancers according to their topography (location)
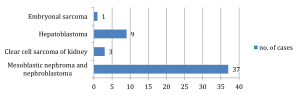
Figure 1: Subtypes of complex mixed and stromal neoplasms
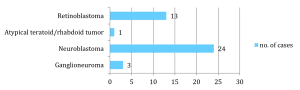
Figure 2: Subtypes of neuroepitheliomatous neoplasms
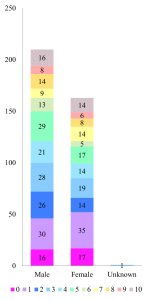
Figure 3: Number of males and females grouped according to age
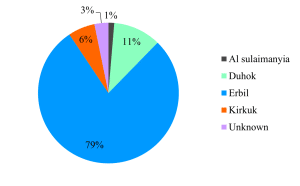
Figure 4: Distribution of the cases among different cities in Kurdistan
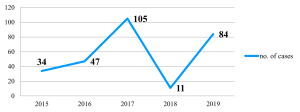
Figure 5: Number of cancer cases diagnosed yearly from 2015 to 2019
Discussion
Our study identified leukemia to be the most common histological type of cancer among children (Table 1). Leukemia accounts for 27% of childhood cancers in the U.S [5], 30% in France and Ireland [6], 33% in Germany [7], and 35% in China [8]. Therefore, our result of 31.8% is consistent with international data. Despite the high incidence of leukemia, the cause of the disease is not known in most cases [9], and there are no prevention programs for childhood leukemia [10]. While the overall long-term event-free survival rate in children with acute leukemia approaches 80%, the incidence increases by an average of 0.7% per year [11].
Among the complex mixed and stromal neoplasms, most cases were mesoblastic nephromas and nephroblastomas (refer to figure 1). While nephroblastoma (also known as Wilms tumor) is said to be the most common pediatric renal cancer overall [12], mesoblastic nephroma is the most common renal neoplasm in the first 3–6 months of life [13]. Due to the high reported rates of renal cancer, it is expected that these neoplasms are one of the most common pediatric cancers in Kurdistan. However, hepatoblastomas have a relatively high incidence compared to other studies. In Western countries, hepatoblastomas comprise 1 percent of cancers below the age of 15 [14]. On the other hand, hepatoblastoma comprised 2.4% of cancers in children below the age of 10 in Kurdistan. The exact cause is unknown; however, there appears to be a strong association between low birth weight and the incidence of hepatoblastoma [15]. A study comparing cancer data with birth weight is needed to determine whether low birth weight is the reason behind the relatively higher incidence of hepatoblastoma in Kurdistan.
The third most common cancer among children in the KRG was found to be lymphomas (both Hodgkin and non-Hodgkin lymphomas). This finding is consistent with the international studies conducted [16]. It is important to analyze the risk factors behind lymphomas, which include a weakened immune system and defects in DNA repair (i.e., ataxia telangiectasia). It is well known that the most common cause of childhood acquired immune deficiency is HIV infection. This link between HIV infection (along with other causes of immune deficiencies, such as malnutrition, etc.) and lymphomas may help explain the unique trend seen in Africa (whereby lymphoma was the most common pediatric malignancy). Fortunately, there are few cases of HIV reported annually in the KRG, Iraq, and this may be one of the reasons that lymphomas are not the most common childhood malignancy in the region. Neuroepitheliomatous neoplasms are primitive neuroectodermal primary peripheral nerve malignancies that occur in bones or soft tissues and tend to manifest aggressive behavior [17]. 57% of the neuroepitheliomatous neoplasm cases were neuroblastomas (Figure 2), making up 6.4% of the total childhood cancers. This result closely resembles cancer rates in the US, where neuroblastomas account for 6% of cancers in ages 0 to 14 [18].
The fifth most common childhood malignancy reported was gliomas, which originate in the glial cells that surround and support neurons in the brain (including astrocytes, oligodendrocytes, and ependymal cells). The term glioma comprises the following subtypes: astrocytomas, brain stem gliomas, ependymomas, and optic nerve gliomas. This finding contradicts international studies, since most of the international studies deduced that brain and other CNS tumors were the most common malignancies following leukemias [19].
In 2017, there were 11.5 million Disability-Adjusted Life Years (DALYs) worldwide (95% uncertainty interval 10³6–12·3) caused by childhood cancer. Among these, 97.3% (97·3–97·3) were attributed to Young’s Lives Losses (YLLs), and 2.7% (2·7–2·7) were considered YLDs. At the global level, childhood cancer ranked as the sixth most significant contributor to the overall cancer burden and the ninth most significant contributor to the burden of childhood diseases. 82·2% (82·1–82·2) of DALYs caused by childhood cancer were found in areas with low, low-middle, or middle Socio-demographic Index. Similarly, 50·3% (50·3–50·3) of the DALYs caused by adult cancer were found in these same categories. Unclassified malignancies in the existing GBD framework accounted for 26·5% (26·5–26·5) of worldwide childhood cancer DALYs [20].
Every year, an estimated 400,000 children and adolescents aged 0-19 years develop cancer. The most diagnosed childhood cancers are leukemias, brain cancers, lymphomas, and solid tumours, like neuroblastoma and Wilms’ tumours. Within high-income countries, where comprehensive services are typically available, the cure rate for children with cancer exceeds 80%. Within low- and middle-income countries (LMICs), the cure rate is below 30%. In general, screening is not effective in preventing or detecting childhood cancer. For the most part, childhood malignancies can be effectively treated with generic drugs and other therapeutic modalities such as surgery and radiation. Medical intervention for childhood cancer can be economically efficient in all socioeconomic contexts. Primary causes of preventable deaths from childhood cancers in LMICs include inadequate diagnosis, incorrect or delayed diagnosis, barriers to receiving treatment, discontinuation of therapy, death due to toxicity, and recurrence. Merely 29% of low-income countries indicate that cancer medications are widely accessible to their populations, in contrast to 96% of high-income countries. The implementation of childhood cancer data systems is essential for facilitating ongoing enhancements in the quality of care and for providing valuable insights for policy planning [21].
Overall, the results of this research proved that there is a slight variation in the incidence pattern of the types of childhood cancers in the Kurdistan Region of Iraq in comparison to the results that were anticipated prior to the start of the research (which stemmed from a review of research done elsewhere in the world). Moreover, the results of this research also varied from the results of the research done in Sulaymaniyah province (2006 to 2014), where the most common types of pediatric cancers were found to be: leukemia, lymphoma, brain, kidney, and bone [4].
One weakness that was present in this research was the fact that the years 2020 and 2021 were not considered due to the unavailability of data. Data over a longer time span would have been more beneficial. Similar studies are needed every few years in order to compare the incidence pattern of childhood cancers in the region with the results acquired from research done in the previous years. Additionally, more detailed statistics regarding factors influencing the cancers (such as risk factors and survival rates) would have provided us with further insight into childhood cancers. Regarding the strengths of the research, it is based on accurate data that has been registered and stored from hundreds of patients. This includes the exact histological types and subtypes, ICD code, anatomical location, behavior, and grade of each cancer diagnosed. Furthermore, the data is highly reliable as it was obtained directly from the official cancer registry department of Kurdistan without any alterations or influence on the data. Lastly, the use of the ICD classification system allows us to compare our results with international data.
Conclusion
Through analysis of data within the Kurdistan region, our study determined the most common cancers in children below 10 years of age. It also provides comparisons with data from other countries, highlighting differences and similarities, which demand further research to identify the cause of these disparities. This includes the high incidence of hepatoblastoma and the low incidence of gliomas. Furthermore, the study highlights the need for more extensive, accurate, and specific data within the KRG, in addition to improved data collection and more organized cancer registries. The study’s results suggest which areas it is most beneficial to direct our limited time and resources into to improve treatment, prevention, and control of cancer in children.
References
- National Cancer Institute. Cancer in children and adolescents. Published 2021. Accessed March 11, 2025. Cancer in Children and Adolescents – NCI
- Miller RW, Young JL Jr, Novakovic B, et al. Childhood cancer. Accessed March 11, 2025. PubMed
- Stefan DC. Patterns of distribution of childhood cancer in Africa. J Trop Pediatr. 2015;61(3):165-173. doi:10.1093/tropej/fmu080 PubMed | Crossref
- Khoshnaw N, Mohammed HA, Abdullah DA. Patterns of cancer in Kurdistan: Results of eight years cancer registration in Sulaymaniyah Province-Kurdistan-Iraq. Asian Pac J Cancer Prev. 2015;16(18):8525-8531. doi:10.7314/apjcp.2015.16.18.8525 PubMed | Crossref | Google Scholar
- Linabery AM, Ross JA. Trends in childhood cancer incidence in the US (1992-2004). Cancer. 2008;112(2):416-432. doi:10.1002/cncr.23257 PubMed | Crossref
- Desandes E, Clavel J, Berger C, et al. Cancer incidence among children in France, 1990-1999. Pediatr Blood Cancer. 2004;43(7):749-757. doi:10.1002/pbc.20145 PubMed | Crossref
- Dreifaldt AC, Carlberg M, Hardell L. Increasing incidence rates of childhood malignant diseases in Sweden during the period 1960-1998. Eur J Cancer. 2004;40(9):1351-1360. doi:10.1016/j.ejca.2004.01.014 PubMed | Crossref
- Bao PP, Zheng Y, Wang CF, et al. Time trends and characteristics of childhood cancer among children age 0-14 in Shanghai. Pediatr Blood Cancer. 2009;53(1):13-16. doi:10.1002/pbc.22042 PubMed | Crossref
- Wiemels J. Perspectives on the causes of childhood leukemia. Chem Biol Interact. 2012;196(3):59-67. doi:10.1016/j.cbi.2012.03.002 PubMed | Crossref
- Metayer C, Dahl G, Wiemels J, Miller M. Childhood leukemia: A preventable disease. Pediatrics. 2016;138(Suppl 1):S45-S55. doi:10.1542/peds.2016-0279 PubMed | Google Scholar
- Pui CH. Acute lymphoblastic leukemia in children. Curr Opin Oncol. 2000;12(1):3-12. doi:10.1097/00001622-200001000-00002 Crossref
- Leslie SW, Sajjad H, Murphy PB. Wilms tumor. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022. Accessed March 11, 2025. PubMed
- McHugh K. Renal and adrenal tumors in children. Cancer Imaging. 2007;7(1):41-51. doi:10.1102/1470-7330.2007.0020 PubMed | Crossref
- Malogolowkin M. Overview of hepatoblastoma. UpToDate. Accessed March 11, 2025. Overview of hepatoblastoma – UpToDate
- Spector LG, Johnson KJ, Soler JT, Puumala SE. Perinatal risk factors for hepatoblastoma. Br J Cancer. 2008;98(9):1570-1573. doi:10.1038/sj.bjc.6604419 PubMed | Crossref
- Johns Hopkins Pediatric Oncology. Lymphoma. Johns Hopkins Medicine. Published 2017. Accessed March 11, 2025. Johns Hopkins Pediatric Oncology | Johns Hopkins Kimmel Cancer Center
- Voss BL, Pysher TJ, Humphrey GB. Peripheral neuroepithelioma in childhood. 1984;54(12):3059-3064. doi:10.1002/1097-0142(19841215)54:12<3059::AID-CNCR2820541202>3.0.CO;2-S PubMed | Crossref | Google Scholar
- Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer Statistics, 2021. CA Cancer J Clin. 2021;71(1):7-33. doi:10.3322/caac.21654 PubMed | Crossref | Google Scholar
- Satyanarayana L, Asthana S, Labani SP. Childhood cancer incidence in India: A review of population-based cancer registries. Indian Pediatr. 2014;51(3):218-220. doi:10.1007/s13312-014-0433-3 PubMed | Crossref | Google Scholar
- GBD 2017 Childhood Cancer Collaborators. The global burden of childhood and adolescent cancer in 2017: An analysis of the Global Burden of Disease Study 2017. Lancet Oncol. 2019;20(9):1211-1225. doi:10.1016/S1470-2045(19)30339-3 PubMed
- World Health Organization. Childhood cancer. Published 2025. Accessed March 11, 2025. Childhood cancer
Acknowledgments
We’re extremely grateful to the Kurdistan Ministry of Health’s Head of Cancer Department (Dr. Chinar Sinjawi) as well as the manager of Awat Radiation Oncology Center (Dr. Bestoon Saifaddin Hassan) for providing the necessary data for our research. We would also like to express our deepest gratitude to our supervisors (Dr. Othman Arab and Dr. Srwa Khalid), who have supported us throughout this research.
Funding
Not reported
Author Information
Corresponding Author:
Darya Y. Mokri
Department of Medicine
University of Kurdistan Hewlêr, Iraq
Email: daryayousefi6@gmail.com
Co-Authors:
Miran D. Salah Al-deen
Department of Medicine
University of Kurdistan Hewlêr, Iraq
Srwa Khalid
Department of Obstetrics & Gynaecology
University of Kurdistan Hewlêr, Iraq
Authors Contributions
All authors contributed to the conceptualization, investigation, and data curation by acquiring and critically reviewing the selected articles. They were collectively involved in the writing – original draft preparation, and writing – review & editing to refine the manuscript. Additionally, all authors participated in the supervision of the work, ensuring accuracy and completeness. The final manuscript was approved by all named authors for submission to the journal.
Ethical Approval
Not reported
Conflict of Interest Statement
Not reported
Guarantor
None
DOI
Cite this Article
Darya YM, Miran DS A-deen, Srwa K. An Insight into the Most Common Cancers in Children Under the Age of 10 Years in Kurdistan, Iraq: A Cross-Sectional Descriptive Study. medtigo J Med. 2024;2(3):e3062246. doi:10.63096/medtigo3062246 Crossref






