Author Affiliations
Abstract
This comprehensive review explores the recent advancements in Enhanced External Counter Pulsation (EECP) therapy, focusing on its underlying mechanisms, clinical effectiveness, and potential future directions. The primary objectives of this review are to elucidate the physiological mechanisms through which EECP exerts its therapeutic effects, assess the current state of clinical evidence supporting its efficacy in various cardiovascular conditions, and provide insights into potential avenues for future research and development.
Methods: A thorough literature review was conducted to gather relevant studies, clinical trials, and experimental investigations related to EECP therapy. The search encompassed electronic databases, medical journals, and conference proceedings, with a focus on recent publications. The retrieved articles were analyzed for insights into the mechanisms of action and clinical outcomes of EECP. Additionally, studies exploring novel applications and future perspectives of EECP were included.
Main Findings: The review synthesizes findings regarding the physiological mechanisms underlying EECP, including its impact on coronary perfusion, vascular function, and neurohormonal regulation. A critical evaluation of clinical studies reveals the efficacy of EECP in managing angina, heart failure, and other cardiovascular conditions. The analysis highlights the positive effects on exercise tolerance, quality of life, and endothelial function. Furthermore, the review discusses emerging research on the potential application of EECP in related fields, such as neurology and pulmonary medicine.
Keywords
Counter pulsation, Coronary artery disease, Heart failure, Myocardial ischemia, Refractory angina.
Introduction
EECP is a non-invasive outpatient therapy used to enhance myocardial perfusion in individuals suffering from chronic stable angina. The EECP machine is composed of various components, such as a machine frame, a driving motor, dual-direction screw rods, a driving bevel gear, driven bevel gears, sliding blocks, a valve body base, charge and exhaust electromagnets, charge and exhaust sleeve cylinders, charge and exhaust ports, charge and exhaust valve elements, and charge and exhaust valve element returning springs [1, 2]. The machine frame serves as the framework for the device, while the driving motor provides the necessary power. The dual-direction screw rods, which are driven by the driving motor, are responsible for propelling the clamping blocks used in the counterpulsation treatment [3]. The sliding blocks are crucial in regulating the movement of the screw rods [4]. Within the valve body base, one can find the charge and exhaust valve components, which include the charge and exhaust electromagnets, charge and exhaust sleeve cylinders, and charge and exhaust valve elements [5]. These components work in tandem to govern the charge and exhaust of air within the device.

Figure 1: EECP Machine
The three inflatable cuffs of the EECP machine are similar to blood pressure cuffs and are tightly secured around the calves, as well as the lower and upper thighs. The patient is attached to a 3-lead ECG cable and finger plethysmography, as shown in Figure 2 and 3. These connections are linked to the touchscreen control console, which continuously monitors the ECG and arterial pressure waveform, as illustrated in Figure 4. The cuffs are promptly and sequentially inflated with utmost accuracy in microseconds, triggered by the ECG mechanism. This inflation commences from the lower calves and progresses towards the upper thighs during the diastolic phase of each cardiac cycle. The pressure within the cuffs, reaching approximately 260-300mmHg, induces a robust arterial compression, thereby stimulating a retrograde flow towards the heart during the closure of the aortic valves. Consequently, this significantly enhances blood flow to the coronary arteries.
Furthermore, the inflation of the cuffs facilitates the retrograde venous blood flow towards the right side of the heart. This, in turn, enables a more substantial ventricular filling and an increased cardiac output [6, 7]. During the presystolic cardiac cycle, when the heart is in the early stage of contraction, all three cuffs deflate simultaneously, thereby considerably reducing the workload of the heart and the myocardial muscle’s demand for oxygen. Diastolic augmentation is the elevation of diastolic pressure achieved through cuff inflation. The degree of diastolic augmentation can be assessed and interpreted by means of the Diastole/Systole Ratio (D/S ratio), which is obtained non-invasively through finger plethysmography. This ratio is measured in terms of two values: the peak amplitude value (P-value) and the area under the curve value (A-value). The system automatically generates these two values when the freeze button on the console is pressed. Alternatively, the values can be manually calculated using the waveform.
The patient is required to undergo a therapy duration of 35 hours, which can be organized as 1 hour per day for 35 days or administered twice daily, depending on the patient’s tolerance.

Figure 2: The patient is attached to a 3-lead ECG cable and finger plethysmography

Figure 3: Applying ECG leads to the patient
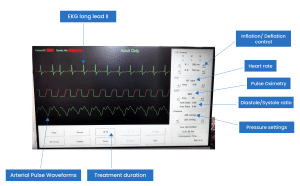
Figure 4: EECP Monitor (Touchscreen Console)
Mechanisms of Action
EECP is an alternative, non-pharmacological, secure intervention that has demonstrated a reduction in angina symptoms, decreased nitrate utilization, increased exercise tolerance, and improvement in myocardial ischemia for patients with refractory angina [8]. This process results in elevated retrograde shear stress of the femoral artery and retrograde-turbulent blood flow, whereas the brachial artery receives increased antegrade-laminar shear stress. These rapid blood flow patterns enable flow-mediated dilatation [9].
Research has shown that EECP improves peripheral arterial flow-mediated dilation and vasoactive substances produced by the endothelium in individuals with symptomatic coronary artery disease. The efficacy of this treatment in alleviating ischemia symptoms is established [10].
Moreover, this therapy has been found to enhance endothelial function and increase the distance at which claudication occurs in peripheral artery disease [11]. Patients with left ventricular dysfunction have reported fewer angina attacks and an overall better quality of life after undergoing EECP, which is supported by research showing a drop in central blood pressure and myocardial oxygen demand [12]. Furthermore, it has been identified as a non-invasive treatment that can restore the functionality of endothelial cells, thereby attenuating hypertensive vascular injury [13]. While medical treatment using antianginal drugs remains the fundamental aspect of therapy, it frequently proves to be inadequate. Therefore, non-pharmacological interventions become necessary. Over the past few decades, various methods have been devised, including pragmatic rehabilitation through cognitive behavioral therapy (CBT), modulation of pain pathways by means of stellate ganglion blockade, and anti-ischemic therapies such as EECP and cardiac sympathetic denervation (CSR) implantation. It is increasingly acknowledged that the most favorable outcomes are attained through combination therapy involving multiple modalities [14].
This treatment has also proven to be cost-effective in reducing hospital expenses for patients with refractory angina [15]. Research has explored the hemodynamic effects of EECP treatment on atherosclerotic plaque in the carotid artery, suggesting its potential clinical application in the management of atherosclerosis [16].
EECP has been recommended for its antiatherogenic properties and has demonstrated efficacy in improving exercise endurance in patients with chronic obstructive pulmonary disease [16, 17].
EECP has been concluded to be a cost-effective adjunctive therapy as well. It has received approval from the US Food and Drug Administration [18]. Some patients undergo EECP therapy multiple times throughout their lifespan as long-term treatment with EECP helps to improve endothelial function significantly, preventing the development of atherosclerotic lesions [18]. Patients with coronary artery disease had improvements in angina pectoris and long-term enhancements in left ventricular function after EECP treatment, attributed to its significant impact on myocardial perfusion [19].
Patients suffering from ischemic left ventricular dysfunction have reported better outcomes after undergoing EECP, which increases exercise capacity and endothelial function [20]. EECP has been observed to enhance vascular function and blood flow in patients with coronary artery disease [21]. Moreover, EECP treatment has been demonstrated to improve the renal function of cardiac patients who are suffering from reduced renal function or elevated NT-proBNP levels [22].
Thus, EECP works by improving endothelial function, renal function, cardiac perfusion, blood flow patterns, and peripheral arterial flow-mediated dilation.
It also demonstrates positive effects on cardiac performance, central blood pressure, and peripheral resistance artery blood flow. These advancements in understanding the physiological mechanisms of EECP highlight its potential as an effective therapy for improving blood flow, vascular function, and cardiac performance in patients with cardiovascular conditions.
Discussion
Clinical Applications and Patient Outcomes
About 620 million people throughout the world deal with heart and circulation issues. This number has been on the rise due to lifestyle changes, aging, a growing population, and better survival rates after cardiovascular diseases. This figure is likely to keep growing if current trends keep up. One out of every thirteen people on Earth is coping with some cardiovascular illness or condition, according to statistics. In 2019, there were more women than men affected by cardiovascular disorders, with 290 million women (or 53% of the total) and 260 million men (or 41% of the total). It is worth noting that over 285 million people throughout the globe were dealing with cardiovascular problems in 1990. By 2010, this number rose to over 430 million, up from to 350 million in 2000. There has been a doubling in the number of people afflicted with cardiovascular diseases since 1997. According to statistical data from 2019, there are 200 million individuals worldwide who suffer from coronary (ischemic) heart disease. Additionally, 110 million people experience peripheral arterial (vascular) disease, 100 million suffer from stroke, and 60 million have atrial fibrillation, making them the next most common cardiovascular conditions. About 60 million people throughout the globe get a heart or circulatory illness diagnosis every year. No other disease kills more people than CAD [23].
Invasive treatment options for unstable angina, myocardial ischemia (both non-ST elevation and ST elevation), and unstable angina include stent implantation and coronary artery bypass graft. However, it has disadvantages such as side effects from medications, complications from procedures, restenosis, and graft attrition. Conventional revascularization techniques may be unsuitable in many circumstances due to patients’ preferences, insufficient distal coronary artery targets, and co-morbidities. Refractory angina pectoris is a diagnosis for people who continue to have symptoms of reduced blood flow to the heart after receiving regular medical therapy and revascularization treatments [24]. EECP has been reported to lead to a significant improvement in the quality of life of patients with coronary artery disease who are not suitable for percutaneous coronary intervention or coronary artery bypass grafting [25].
Importantly, meta-analyses have shown the safety and effectiveness of EECP in patients with refractory angina, leading to improvements in treatment efficacy [26]. According to research, EECP may improve exercise capacity and overall quality of life for those dealing with chronic heart failure (CHF) [27].
In addition, EECP has been investigated in the treatment of erectile dysfunction, exhibiting potential in alleviating symptoms [28]. EECP has received approval from the Food and Drug Administration (FDA) for the management of stable angina and has been shown to reduce the severity of angina and improve exercise tolerance effectively [29]. As a result, EECP has shown promise in improving exercise tolerance and reducing endothelial dysfunction in CAD patients [30]. Additionally, systematic reviews and meta-analyses have indicated that EECP can improve symptoms of angina, myocardial ischemia, left ventricular function, and overall quality of life, thereby highlighting its long-term benefits [31]. Furthermore, experts have endorsed the clinical application of EECP in the elderly population, emphasizing its potential in managing various comorbidities, including angina and heart failure [32]. Overall, EECP has emerged as a non-invasive and effective treatment modality for various cardiovascular conditions, offering potential advantages in improving patient outcomes.
EECP treatment significantly improves breathlessness, walking distance in six minutes, and ejection fraction in heart failure patients. The treatment also significantly decreases serum urea and LDL levels. These positive changes may be attributed to a sudden increase in cardiac output and hyperdynamic circulation during the treatment [32].
Recent Advancements
Recent technological advancements in EECP therapy have made significant contributions to its effectiveness, accessibility, and impact on patient experience. These advancements primarily focus on enhancing treatment precision and customization through the application of patient-specific computational fluid dynamics analysis. As a result, the hemodynamic effects are improved, and endothelial functions are enhanced [16].
In a randomized clinical trial conducted by Sharma et al., the protocol explores the utilization of EECP in patients suffering from symptomatic and severe intracranial steno-occlusive disease. This study suggests the potential extension of EECP applications beyond traditional cardiovascular conditions. The study objective was to evaluate the efficacy of Enhanced External Counter Pulsation therapy in patients with severe stenosis of the intracranial internal carotid (ICA) or middle cerebral artery (MCA) experiencing symptomatic and severe intracranial steno-occlusive disease. The primary aim of their study was to assess whether EECP therapy, known for its ability to improve myocardial perfusion by promoting collateral blood vessel development in the heart, can also provide benefits for patients with severe intracranial stenosis. The authors concluded that EECP, as a novel non-invasive therapeutic intervention, has the potential to assist a larger number of patients in preventing ischemic events and reducing the burden of stroke [33].
Chen et al.’s study on treatment strategies utilizing different frequencies of EECP for coronary heart disease and cerebral ischemic stroke introduces a nuanced approach to tailoring EECP therapy based on the specific condition. It emphasizes the importance of personalized treatment plans [34].
Recent technological advancements in the field of EECP have resulted in the development of more compact and portable devices that can be integrated into clothing, enabling patients to remain mobile during treatment. Additionally, the utilization of complex pulse sequences and the treatment of various conditions, such as cognitive disorders, diabetes, and renal disease, have been mentioned. However, specific recent technological innovations related to ECCP therapy are not explicitly addressed. These innovations strive to enhance the convenience and effectiveness of external counter-pulsation therapy, offering patients the benefits of exercise without the strain and difficulties associated with conventional cardiovascular exercise routines [35].
EECP therapy has shown promise in improving a range of conditions, such as intracranial stenosis, chronic heart failure, and venous diseases.
In comparison, EECP has demonstrated encouraging long-term benefits in enhancing patient outcomes and quality of life when compared to other therapeutic interventions. These benefits include improvements in exercise capacity, anginal symptoms, myocardial ischemia, left ventricular function, and overall quality of life, which are not consistently observed with other treatment modalities.
Challenges and Limitations
One of the limitations is that EECP therapy is primarily focused on managing chronic stable angina (CSA) and may not demonstrate effectiveness for all patients with CSA, as its efficacy varies, and further research is required to determine its economic worth [35]. Additionally, although EECP appears to be a safe and well-tolerated treatment option for patients with refractory angina pectoris (RAP), there may still be adverse effects associated with the therapy, such as muscle pain/soreness and bradycardia [36]. Moreover, EECP treatment may not be appropriate for all patients, as it is predominantly studied in individuals aged 80 years and older who have coronary heart disease [37].
Furthermore, further investigation is required to evaluate the long-term effectiveness and safety of combining EECP with other treatments, such as sacubitril/valsartan, in patients with chronic heart failure [38]. Concerning venous diseases, ongoing research aims to assess the effects of EECP on symptoms and quality of life, particularly in reducing swelling and night cramps [39]. Overall, continuous research and advancements in EECP therapy possess the potential to address these challenges and further improve patient outcomes.
Future Perspectives
Enhanced external counterpulsation (EECP) has exhibited promise in the management of ischemic cardiovascular and cerebrovascular diseases. Recent research has focused on the potential advancements and emerging technologies that may impact the future of EECP. These findings have led to the development of a new model of EECP equipment that may serve not only in secondary, but also primary prevention of atherosclerotic disease [40].
Apart from treating the angina or CAD, EECP has shown promising benefits in other conditions as well. The depression showed better following EECP therapy. May et al. studied 50 patients with angina of CCS class II or higher who underwent EECP therapy for over a year. They found a significant decrease in major depression inventory scores, indicating a statistically meaningful improvement in depressive symptoms lasting beyond one year [41].
Compelling evidence was observed in patients with angina and heart failure who also had other concurrent conditions, including restless leg syndrome [42].
Enhanced penile function has been noted in patients with and without persistent refractory angina following EECP therapy. Thus, it also improved erectile dysfunction [43, 44].
Other conditions that showed positive effects after undergoing EECP were nonarteritic ischemic optic neuropathy [45], syndrome X [46], and hepatorenal syndrome [47].
With an older population and a general downward trend in the use of invasive revascularization operations for CAD, EECP therapy has the potential to become more widely used in the future due to the data supporting its usage as a non-invasive, low-cost therapeutic option. Further research should continue to expand the understanding of the intricate mechanisms that contribute to the effectiveness of this innovative therapy.
Expanding the scope of EECP could allow it to be utilized for many illnesses beyond heart failure and angina caused by CAD, such as those stemming from systemic endothelial dysfunction and inflammation [48].
Thus, EECP treatment has been shown to boost the recruitment of collateral circulation and enhance endothelial function, which may be the most promising and advantageous effects of EECP treatment. Further research in these areas may lead to advancements in EECP technology and its clinical application in the future.
Moreover, ongoing research is required to address potential areas for improvement, such as optimizing treatment protocols and identifying patient populations that would benefit the most from EECP. In the future, EECP therapy is expected to continue evolving with potential advancements in precision medicine, personalized treatment protocols, and emerging technologies that may further enhance its efficacy and long-term benefits. Research areas may focus on refining patient selection criteria, optimizing treatment protocols, and exploring the potential synergistic effects of EECP with other therapeutic modalities to maximize its long-term benefits.
Conclusion
In conclusion, this review provides a comprehensive overview of the current understanding of EECP therapy, emphasizing its multifaceted mechanisms and proven clinical benefits. The findings underscore the therapeutic potential of EECP in cardiovascular medicine while also identifying areas for future investigation. By shedding light on the evolving landscape of EECP research, this review aims to guide clinicians, researchers, and policymakers in shaping the future trajectory of this non-invasive therapeutic modality.
References
- Liu H, Liang H, Yu X, Wang G, Han Y, Yan M, Li S, Wang W. Enhanced external counterpulsation modulates the heartbeat evoked potential. Front Physiol. 2023;14:1144073. doi.10.3389/fphys.2023.1144073
PubMed | Crossref | Google Scholar - Xie Z. External counter pulsation device based on dual-direction roller screw rods. PatSnap. 2019. External counter pulsation device based on dual-direction roller screw rods
- Chen Z, Li X. Charge and exhaust valve for enhanced external counter pulsation. PatSnap. 2017. Charge and exhaust valve for enhanced external counter pulsation.
- Liu H, Liang H, Yu X, Han Y, Wang G, Yan M, Wang W, Li S. A study on the immediate effects of enhanced external counter pulsation on physiological coupling. Front Neurosci. 2023;7:17:1197598. doi.10.3389/fnins.2023.1197598 PubMed | Crossref | Google Scholar
- Li B, Wang W, Mao B, Zhang Y, Chen S, Yang H, Niu H, Du J, Li X, Liu Y. Hemodynamic effects of enhanced external counter pulsation on cerebral arteries: A multiscale study. Biomed Eng Online. 2019;18(1):91. doi.10.1186/s12938-019-0710-x PubMed | Crossref | Google Scholar
- Stys T, Lawson WE, Hui JCK, Lang G, Liuzzo J, Cohn PF. Acute hemodynamic effects and angina improvement with enhanced external counter pulsation. Am Heart J. 2001;152(10):653-658. doi.10.1177/000331970105201001 PubMed | Crossref | Google Scholar
- Suresh K, Simandl S, Lawson WE, Hui JCK, Lo L, Burger L, Cohn PF. Maximizing the hemodynamic benefit of enhanced external counterpulsation. Clin Cardiol. 1998;21(9):649-653. doi.10.1002/clc.4960210908
PubMed | Crossref | Google Scholar - Cáceres J, Atal P, Arora R, Yee D. Enhanced external counterpulsation: a unique treatment for the “no‐option” refractory angina patient. J Clin Pharm Ther. 2021;46(2):295-303. doi.10.1111/jcpt.13330 PubMed | Crossref | Google Scholar
- Gurovich A, Braith R. Enhanced external counterpulsation creates acute blood flow patterns responsible for improved flow-mediated dilation in humans. Hypertens Res. 2012;36(4):297-305. doi.10.1038/hr.2012.169 PubMed | Crossref | Google Scholar
- Braith R, Conti C, Nichols W, Choi C, Khuddus M, Beck D, Casey D. Enhanced external counter pulsation improves peripheral artery flow-mediated dilation in patients with chronic angina. Circulation. 2010;122(16):1612-1620. doi.10.1161/CIRCULATIONAHA.109.923482 PubMed | Crossref | Google Scholar
- Buschmann E, Brix M, Li L, Janke D, Zietzer A, Li M, Hillmeister P. Adaptation of external counter pulsation based on individual shear rate therapy improves endothelial function and claudication distance in peripheral artery disease. Vasa. 2016;45(4):317-324. doi.10.1024/0301-1526/a000544 PubMed | Crossref | Google Scholar
- Beck D, Casey D, Martin J, Sardina P, Braith R. Enhanced external counter pulsation reduces indices of central blood pressure and myocardial oxygen demand in patients with left ventricular dysfunction. Clin Exp Pharmacol Physiol. 2015;42(4):315-320. doi.10.1111/1440-1681.12367 PubMed | Crossref | Google Scholar
- Liang J, Shi J, Wei W, Wu G. External counterpulsation attenuates hypertensive vascular injury through enhancing the function of endothelial progenitor cells. Front Physiol. 2021;11:590585. doi.10.3389/fphys.2020.590585 PubMed | Crossref | Google Scholar
- Ali N, Patel P. Non-pharmacological interventions in refractory angina. Heart Res Open J. 2018;5(1):1-7. doi.10.17140/HROJ-5-146 Crossref
- Lawson W, Hui J, Kennard E, Linnemeier G. Enhanced external counter pulsation is cost-effective in reducing hospital costs in refractory angina patients. Clin Cardiol. 2015;38(6):344-349. doi.10.1002/clc.22395 PubMed | Crossref | Google Scholar
- Du J, Wu G, Wu B, Liu C, Mai Z, Liu Y, Wang Y, Zhang P, Liu J. The hemodynamic effect of enhanced external counter pulsation treatment on atherosclerotic plaque in the carotid artery: a framework of patient-specific computational fluid dynamics analysis. Front Physiol. 2020: 5903790. doi.10.1155/2020/5903790 PubMed | Crossref | Google Scholar
- Zhao M, Huang Y, Lian L, Zhou L, Wu Z, Liu Y, Zhang H. Enhanced external counterpulsation efficacy on exercise endurance in COPD patients and healthy subjects: a pilot randomized clinical trial. Int J Chron Obstruct Pulmon Dis. 2020;15:25-31. doi.10.2147/COPD.S225566 PubMed | Crossref | Google Scholar
- Yin Y, He Q, Zhang R, Cheng H, Zhang Y, Zhang J. Predictors of adherence of enhanced external counter pulsation in patients with coronary heart disease after discharge: a mixed-methods study. Front Cardiovasc Med. 2022;9:1005958 doi.10.3389/fcvm.2022.1005958 PubMed | Crossref | Google Scholar
- Qin X, Deng Y, Wu D, Yu L, Huang R. Does enhanced external counterpulsation (EECP) significantly affect myocardial perfusion?: a systematic review and meta-analysis. PLoS One. 2016;11(4):e0151822. doi.10.1371/journal.pone.0151822. PubMed | Crossref | Google Scholar
- Beck D, Martin J, Casey D, Avery J, Sardina P, Braith R. Enhanced external counterpulsation improves endothelial function and exercise capacity in patients with ischemic left ventricular dysfunction. Clin Exp Pharmacol Physiol. 2014;41(9):628-636. doi.10.1111/1440-1681.12263 PubMed | Crossref | Google Scholar
- Avery J, Beck D, Casey D, Sardina P, Braith R. Enhanced external counterpulsation improves peripheral resistance artery blood flow in patients with coronary artery disease. Appl Physiol Nutr Metab. 2014;39(3):405-408. doi.10.1139/apnm-2013-0309 PubMed | Crossref | Google Scholar
- Ruangkanchanasetr P, Mahanonda N, Raungratanaamporn O, Ruckpanich P, Kitiyakara C, Chaiprasert A, Supaporn T. Effect of enhanced external counterpulsation treatment on renal function in cardiac patients. BMC Nephrol. 2013;14:193. doi.10.1186/1471-2369-14-193 PubMed | Crossref | Google Scholar
- British Heart Foundation. Global heart and circulatory diseases factsheet 2025. Global heart and circulatory diseases factsheet
- Rajendra KV. Enhanced counter-pulsation therapy: a non-invasive treatment modality for cardiovascular patients. J Clin Res Appl Med. 2022;2(2):19-20. doi.10.5530/jcram.2.2.6 Crossref
- Shen L, Wang X, Wu G. Expert consensus on the clinical application of enhanced external counterpulsation in elderly people (2019). Aging Med. 2020;3(1):16-24. doi.10.1002/agm2.12097 PubMed
- Rayegani S, Heidari S, Maleki M, Seyed-Nezhad M, Heidari M, Parhizgar S, Moradi-Joo M. Safety and effectiveness of enhanced external counterpulsation (EECP) in refractory angina patients: a systematic review and meta-analysis. J Cardiovasc Thorac Res. 2021;13(4):265-276. doi.10.34172/jcvtr.2021.50 PubMed | Crossref | Google Scholar
- Zhou Z, Wang D, Li X, Zhang C, Wu C. Effects of enhanced external counterpulsation on exercise capacity and quality of life in patients with chronic heart failure. Medicine (Baltimore). 2021;100(27):e26536. doi.10.1097/MD.0000000000026536. PubMed | Crossref | Google Scholar
- Raeissadat S, Javadi A, Allameh F. Enhanced external counterpulsation in rehabilitation of erectile dysfunction: a narrative literature review. Vasc Health Risk Manag. 2018;14:393-399. doi.10.2147/VHRM.S181708. PubMed | Crossref | Google Scholar
- Rezapour A, Naghdi S, Ghiasvand H, Moradi T, Kabir MJ, Yousefzadeh N. A systematic review on the economic evaluations evidence of enhanced external counter-pulsation (EECP) for managing chronic stable angina. Med J Islam Repub Iran. 2022;36:100. doi.10.47176/mjiri.36.100 PubMed | Crossref | Google Scholar
- Yang H, Song L, Ning X, Ma Y, Xue A, Zhao H, Du Y, Lu Q, Liu Z, Wang J. Enhanced external counterpulsation ameliorates endothelial dysfunction and elevates exercise tolerance in patients with coronary artery disease. Front Cardiovasc Med. 2022;9:997109. doi.10.3389/fcvm.2022.997109. PubMed | Crossref | Google Scholar
- Jan R, Khan A, Zahid S, Sami A, Owais SM, Khan F, Asjad SJ, Jan MH, Awan ZA. The effect of enhanced external counterpulsation (EECP) on quality of life in patients with coronary artery disease not amenable to PCI or CABG. Cureus. 2020;12(5):e7987. doi.10.7759/cureus.7987. PubMed | Crossref | Google Scholar
- Subramanian R, Shiek A, Meyyappan C. Efficacy of enhanced external counterpulsation in improving six minutes’ walk test in heart failure patients. Biomedicine (Taipei). 2022;42(2):68 doi.10.51248/.v42i2.1224 Crossref
- Sharma VK, Gopinathan A, Tan BYQ, et al. Enhanced external counterpulsation therapy in patients with symptomatic and severe intracranial steno-occlusive disease: A randomized clinical trial protocol. Front Neurol. 2023;14:1177500 doi.10.3389/fneur.2023.1177500 PubMed | Crossref | Google Scholar
- Chen M, Liu Y, Xu K, et al. Treatment strategy of different enhanced external counterpulsation frequencies for coronary heart disease and cerebral ischemic stroke: A hemodynamic numerical simulation study. SSRN. 2023:39:107640 doi.10.1016/j.cmpb.2023.107640. PubMed
- Poon M. External counter pulsation system. FPO. 2020. External counter pulsation system
- Verma RK. Enhanced counter-pulsation therapy: A non-invasive treatment modality for cardiovascular patients. J Clin Res Appl Med. 2022;2(2):19-20. doi.10.5530/jcram.2.2.6 Crossref
- Rezapour A, Naghdi S, Ghiasvand H, et al. A systematic review on the economic evaluations evidence of enhanced external counter-pulsation (EECP) for managing chronic stable angina. Med J Islam Repub Iran. 2022;36:100 PubMed | Crossref | Google Scholar
- Wu E, Wu E, Mårtensson J, et al. Adverse events and their management during enhanced external counterpulsation treatment in patients with refractory angina pectoris: Observations from a routine clinical practice. Eur J Cardiovasc Nurs. 2021;21(2):152-160. doi.10.1093/eurjcn/zvab040. PubMed | Crossref | Google Scholar
- Huang XL, Wang XJ, Chen BT, Chen YN. Clinical efficacy of enhanced external counterpulsation plus sacubitril/valsartan in the treatment of patients with chronic heart failure and the effect on ankle-arm index and cardiac function. Eur Rev Med Pharmacol Sci. 2023;27(8):3300-3312. doi.10.26355/eurrev_202304_32101 PubMed
- Feldman AM. Enhanced external counter pulsation: Mechanism of action. Clin Cardiol. 2007;25(Suppl 2):11-15. doi.10.1002/clc.4960251405 PubMed
- May O, Søgaard HJ. Enhanced external counterpulsation is an effective treatment for depression in patients with refractory angina pectoris. Prim Care Companion CNS Disord. 2015;17(4):10.4088/PCC.14m01748. doi.10.4088/PCC.14m01748 PubMed | Crossref | Google Scholar
- Rajaram SS, Shanahan J, Ash C, et al. Enhanced external counter pulsation (EECP) as a novel treatment for restless legs syndrome (RLS): A preliminary test of the vascular neurologic hypothesis for RLS. Sleep Med. 2005;6(2):101-106. doi.10.1016/j.sleep.2004.10.012 PubMed | Crossref | Google Scholar
- Froschermaier SE, Werner D, Leike S, et al. Enhanced external counter pulsation as a new treatment modality for patients with erectile dysfunction. Urol Int. 1998;61(3):168-171. doi.10.1159/000030315 PubMed | Crossref | Google Scholar
- Lawson WE, Hui JC, Kennard ED, et al.; IEPR Investigators. Effect of enhanced external counterpulsation on medically refractory angina patients with erectile dysfunction. Int J Clin Pract. 2007;61(5):757-762. doi.10.1111/j.1742-1241.2007.01328.x PubMed | Crossref | Google Scholar
- Zhu W, Liao R, Chen Y, et al. Effect of enhanced extracorporeal counterpulsation in patients with non-arteritic anterior ischemic optic neuropathy. Graefes Arch Clin Exp Ophthalmol. 2015;253(1):127-133. doi.10.1007/s00417-014-2823-z PubMed | Crossref | Google Scholar
- Kronhaus KD, Lawson WE. Enhanced external counterpulsation is an effective treatment for Syndrome X. Int J Cardiol. 2009;135(2):256-257. doi.10.1016/j.ijcard.2008.03.022 PubMed | Crossref | Google Scholar
- Werner D, Trägner P, Wawer A, et al. Enhanced external counterpulsation: A new technique to augment renal function in liver cirrhosis. Nephrol Dial Transplant. 2005;20(5):920-926. doi.10.1093/ndt/gfh755
PubMed | Crossref | Google Scholar - Raza A, Steinberg K, Tartaglia J, et al. Enhanced external counter pulsation therapy. Cardiol Rev. 2016;1. Enhanced external counter pulsation therapy
Acknowledgments
Not applicable
Funding
Not applicable
Author Information
Independent Researcher, Department of Content
medtigo India Pvt Ltd, Pune, India
Author Contribution
The author contributed to the conceptualization, investigation, and data curation by acquiring and critically reviewing the selected articles and was involved in the writing – original draft preparation and writing – review & editing to refine the manuscript.
Informed Consent
Not applicable
Conflict of Interest Statement
Not applicable
Guarantor
Not applicable
DOI
Cite this Article
Hiremath S. Advances in Enhanced External Counter Pulsation Therapy: Mechanisms, Clinical Efficacy, and Future Perspectives. medtigo J Med. 2023;1(4):e3062141. doi:10.63096/medtigo3062141 Crossref









