Author Affiliations
Abstract
Background: Hernias, whether primary or recurrent, remain a significant surgical challenge, particularly in resource-limited settings. The choice of repair techniques and mesh placement critically influences postoperative outcomes and recurrence risk. This study evaluates the clinical outcomes of open onlay premuscular meshplasty and hybrid repairs in primary, recurrent, and recurrent hernias.
Methodology: A retrospective observational study of 53 adults who underwent open or hybrid abdominal wall hernia repair with mesh between April 2013 and January 2025 was conducted. Patients with incomplete data, major concurrent surgeries, or immunocompromised states were excluded. Demographic, intraoperative, and postoperative data were analyzed using IBM SPSS Statistics 26. Continuous variables were expressed as mean ± SD, and categorical variables as frequencies or percentages. Statistical tests included Chi-square, Fisher’s exact, Student’s t-test, and ANOVA, with p < 0.05 considered significant. Mean follow-up was 12 months.
Results: The mean patient age was 48.62 ± 15.00 years (range 18 to 78 years), with 33 (62.26%) females and 19 (35.85%) males. The mean BMI was 32.03 ± 6.02 (p = 0.021). Primary hernias comprised 28 (52.82%), recurrent 11 (20.76%), and recurrent 14 (26.42%) (p = 0.037). Most repairs were open in 47 (88.68%), using 30×30 cm mesh in 27 (50.94%) (p = 0.029). Mean hospital stay was 2.09 ± 1.12 days, and mean drain duration was 9.56 ± 7.34 days. Complications were minimal, with wound complications in 3 (5.66%). No mesh infections, recurrences, or mortality occurred during follow-up.
Conclusion: Standardized open and hybrid mesh repair techniques demonstrated favorable short-term and 12-month outcomes with low complication rates, excellent cosmetic results, and zero recurrence.
Keywords
Primary hernia, Recurrent hernia, Open onlay premuscular meshplasty, Abdominoplasty, Mesh explantation, Seroma, Hematoma, Flap necrosis, Marginal skin necrosis.
Introduction
Out of primary, recurrent, and recurrent hernias, incisional and ventral hernia repairs remain a significant surgical challenge with recurrence and recurrence, while postoperative morbidity continues to be a key concern despite advances in operative techniques and prosthetic materials. Mesh reinforcement has become the standard of care, with onlay, inlay, and sublay approaches being the most widely practiced techniques (Figure 1).[1,2] Recent systematic reviews and meta-analyses have highlighted ongoing debate regarding the optimal placement of mesh with sublay, often demonstrating lower recurrence and infection rates, while onlay repair remains technically simpler and widely applicable, particularly in resource-limited settings.[3-6] The choice of surgical approach is further complicated in recurrent and recurrent hernia repairs, where altered anatomy, dense adhesions, and layers in which previous mesh implantation increases operative difficulty and risk of complications. Current literature emphasizes that recurrence after incisional hernia repair poses a distinct clinical problem requiring careful patient selection and individualized operative planning.[7,8] Our study evaluates patient demographics, preoperative characteristics, intraoperative variables, and postoperative outcomes in a single-center cohort of 53 patients undergoing primary, recurrent, or re-recurrent hernia repair between April 2013 and January 2025. By systematically analyzing outcomes, including complication rates, cosmetic results, and recurrence patterns, this study aims to evaluate the demographic profile, preoperative characteristics, intraoperative variables, and postoperative outcomes of patients undergoing primary, recurrent, or re-recurrent hernia repair over a 12-year period at a single tertiary care center. Specifically, the study sought to assess complication rates, length of hospital stays, recurrence, and cosmetic outcomes, while analyzing associations between patient factors, surgical techniques, and clinical results using statistical methods.
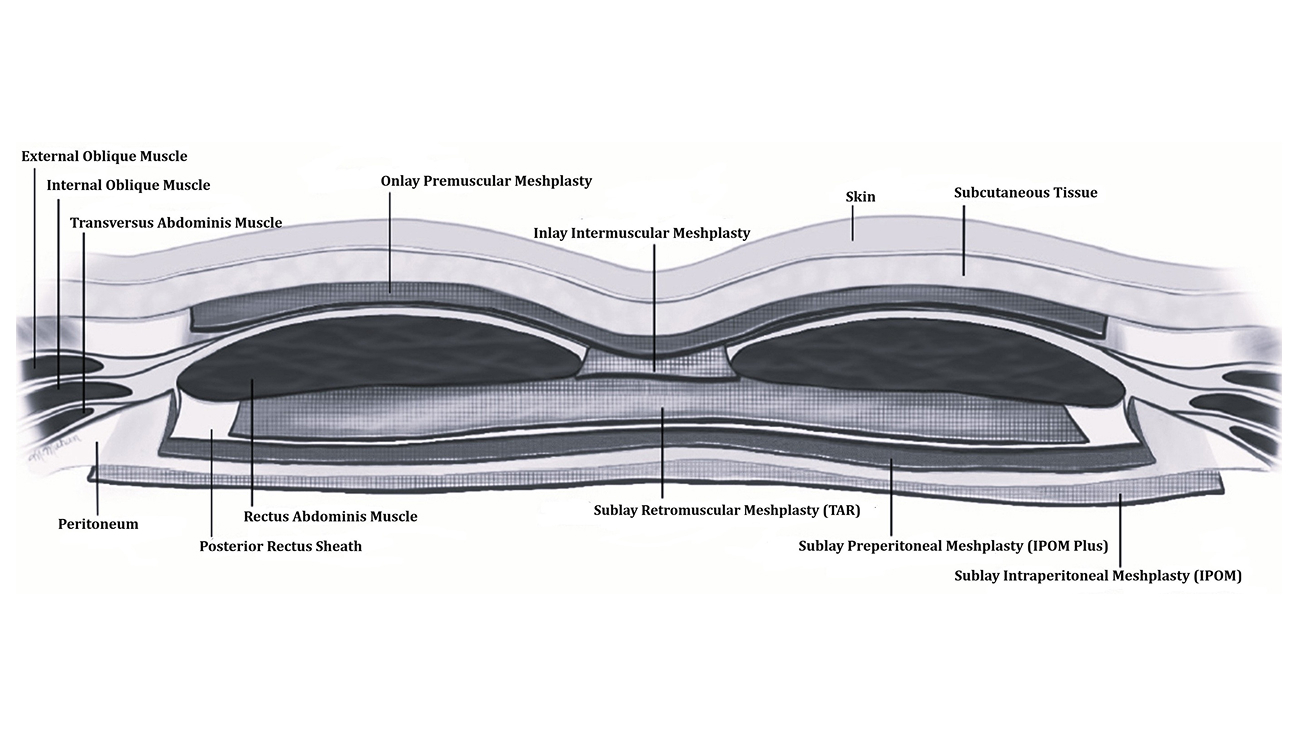
Figure 1: Different planes for hernia repair
Methodology
We prefer the open onlay premuscular meshplasty technique with the patient in the supine position. The choice of anesthesia depends on the case and may include regional blocks, spinal anesthesia, or general anesthesia. The incision site for primary hernia repair varies based on the type and location of the hernia. In cases of recurrent or re recurrent hernias, surgical access often requires reopening the previous incision site or performing a suprapubic pfannenstiel incision with mesh explantation if required for previous meshplasty. For patients undergoing surgery for recurrent or recurrent hernias, we typically recommend the use of an abdominal binder postoperatively for at least 3 to 6 months to support healing and reduce the risk of further recurrence. In our study, we include umbilical hernias, inguinal hernias, epigastric hernias, and divarication of recti as primary hernia repairs. Hernia recurrences, whether following previous repairs or arising after abdominal surgeries (laparoscopic or open) such as appendicectomy, cholecystectomy, renal procedures, laparotomies, or previous failed hernia surgery, are classified and treated as recurrent hernias. Prior to surgery, we ensure comprehensive photographic and video documentation of the hernia pathology, with all patients’ identifying information concealed. Patients and their attendants are given thorough counseling, and we obtain both written and video consent before proceeding. Once consent is secured, the patient is brought to the operating table and placed in the supine position under appropriate regional, spinal, or general anesthesia. The incision site depends on the location and type of hernia (Figure 2a, 2b, 2c).
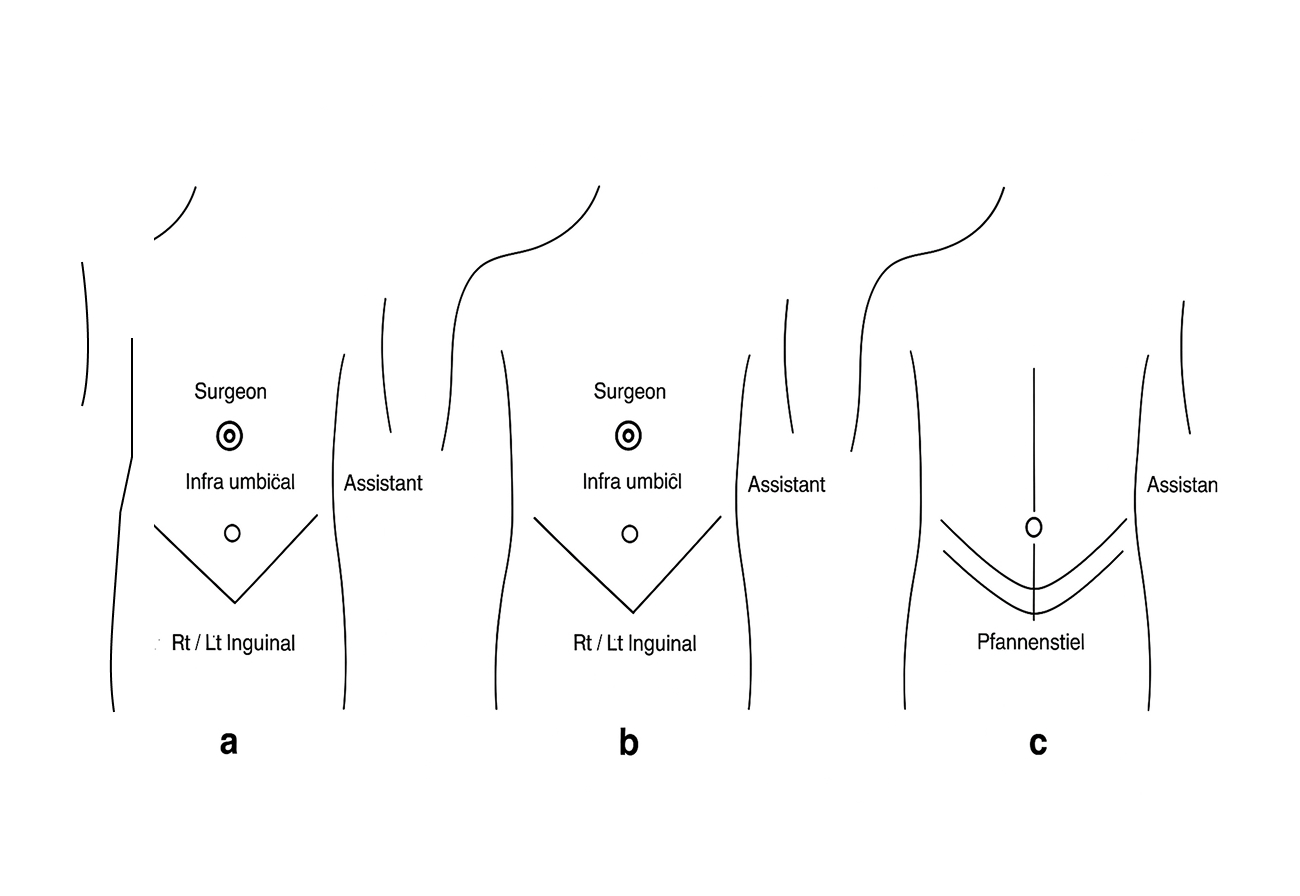
Figure 2: Incision sites
2a: Incision sites for primary hernia
2b: Incision sites for recurrent hernia
2c: Incision sites for recurrent hernia
In primary hernia repair, patients are generally discharged on the same day or the following day with the drain in place for home care. Follow-up visits involve drain removal once output ceases and suture removal between the 8th and 10th postoperative day. While in recurrent and re-recurrent hernia repair, patients are typically discharged the day after surgery with a drain. On follow-up, the drain is removed once output ceases or kept a little longer if required, and sutures are removed on the 12th to 14th postoperative day. Patients are advised to wear an abdominal binder for at least 3 to 6 months and to avoid strenuous activity.
Summary of the techniques:
Photo and video documentation is conducted to confirm the results:
- Pre-operative (Figure 3a, 3b)
- Intra-operative (Figure 3c, 3d)
- Immediate post-operative (Figure 3e)
- At the time of drain and suture removal
- At the one-month post-operative (Figure 3f, 3g)
Drain removal: Usually between the 5th and 14th postoperative day, depending on drain output. Once ceased, if required, a little bit delayed
Suture removal: Performed between the 8th and 14th postoperative day
Abdominal binder: Mandatory for 3 to 6 months postoperatively
Strenuous activity: Should be strictly avoided during the recovery period, at least for 6 months
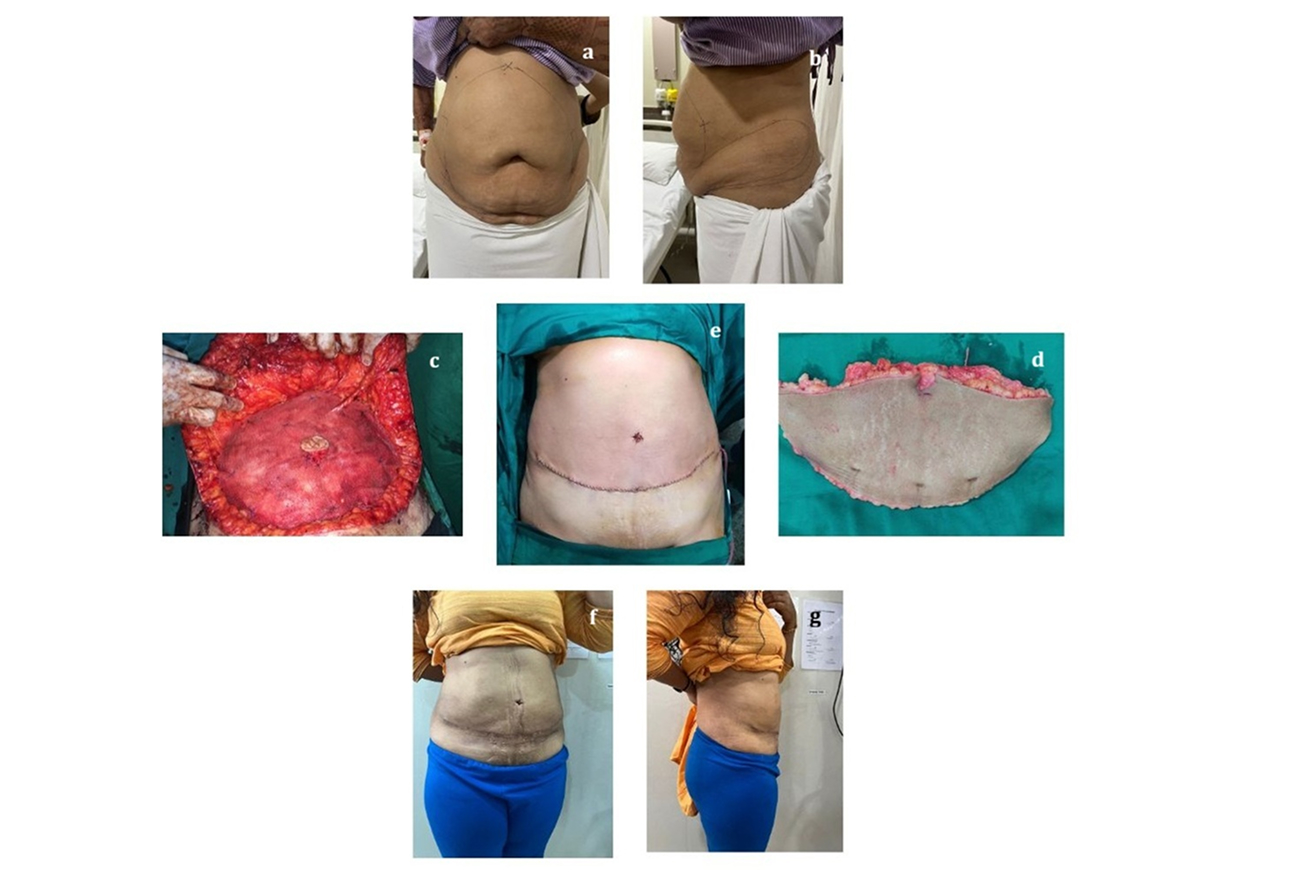
Figure 3: Results
3a: Pre-operative front view
3b: Pre-operative lateral view
3c: Intraoperative meshplasty
3d: Specimen of excision of sagged skin
3e: Immediate postoperative front view
3f: Post-operative front view
3g: Post-operative lateral view
Benefits: Open onlay premuscular hernia repair is delivering favourable cosmetic outcomes and low complication rates compared to other approaches such as open inlay, laparoscopic inlay, open sublay, laparoscopic sublay, and laparoscopic onlay techniques such as Total extra peritoneal hernia repair (TEP), Enhanced transabdominal preperitoneal hernia repair (E TAP), Transabdominal preperitoneal hernia repair (TAPP), Transversus abdominis release (TAR), Intraperitoneal onlay mesh repair (IPOM), Intraperitoneal onlay mesh Plus hernia repair (IPOM Plus), Subcutaneous onlay laparoscopic approach (SCOLA) etc. For primary hernia repairs, this method is often suitable as a day care procedure, while in recurrent or recurrent cases, the postoperative hospital stay is typically limited to 2 to 3 days postoperatively. This method not only strengthens the anterior abdominal wall but also enhances the abdominal contour by enabling the removal of excess sagging skin, all with minimal complications and a shorter recovery period. Such cosmetic refinements, including umbilical repositioning and the removal of excess sagging skin, are not feasible with conventional laparoscopic techniques. In these cases, a hybrid approach may be required, which is generally more time-consuming. Overall, this technique significantly improves the patient’s self-confidence and aesthetic appearance with minimal complications.
Results
| Total number of patients | 53 | April 2013 to January 2025 |
| Age | 18 to 78 years | Mean 48.62±15.00 years |
| Gender distribution | Male: 19
Female: 33 Other: 1 |
35.85%
62.26% 1.89% |
| Body mass index | 23.19-47.27 | Mean 32.03±6.02 |
| Less than 25 | 4 | 7.55% |
| 25 to 30 | 18 | 33.96% |
| 30 to 35 | 17 | 32.08% |
| 35 to 40 | 8 | 15.09% |
| More than 40 | 6 | 11.32% |
Table 1: Demographic characteristics
| Preoperative diagnostic investigations | ||
| Ultrasound | 52 | 98.11% |
| Ultrasound with Computerized Tomography | 1 | 1.89% |
| Preoperative pain duration in days | ||
| No pain | 6 | 11.32% |
| 0 to 30 | 15 | 28.31% |
| 30 to 60 | 8 | 15.09% |
| 60 to 90 | 6 | 11.32% |
| 90 to 120 | 5 | 9.43% |
| More than 120 | 13 | 24.53% |
| Preoperative hernia duration in months | ||
| 0 to 12 | 9 | 16.98% |
| 12 to 24 | 5 | 9.44% |
| 24 to 36 | 9 | 16.98% |
| More than 36 | 30 | 56.60% |
| Hernia presentation | ||
| Primary | 28 | 52.82% |
| Recurrent | 11 | 20.76% |
| Re recurrent | 14 | 26.42% |
Table 2: Preoperative data
| Surgical approach | ||
| Open | 47 | 88.68% |
| Hybrid | 6 | 11.32% |
| Mesh size in cm | ||
| 6×11 | 14 | 26.42% |
| 15×15 | 12 | 22.64% |
| 30×30 | 27 | 50.94% |
| Anaesthesia | ||
| Spinal anaesthesia | 18 | 33.96% |
| General anaesthesia | 32 | 60.38% |
| Spinal with general anesthesia | 3 | 5.66% |
Table 3: Intraoperative data
| Post-operative stays in the hospital in days | ||
| Mean | 2.09±1.12 Days | |
| 1 | 19 | 35.85% |
| 2 | 19 | 35.85% |
| 3 | 9 | 16.98% |
| More than 3 | 6 | 11.32% |
| Drain keeping duration in days | ||
| Mean | 9.56±7.34 Days | |
| No drain | 11 | 20.76% |
| 0 to 7 | 9 | 16.98% |
| 8 to 14 | 20 | 37.74% |
| 15 to 21 | 10 | 18.86% |
| 22 to 28 | 3 | 5.66% |
Table 4: Postoperative data
| Post-operative breathlessness | ||
| Not seen | 48 | 90.57% |
| Mild | 5 | 9.43% |
| Post-operative pain | ||
| Mild | 39 | 73.58% |
| Moderate | 14 | 26.42% |
| Post-operative wound complications | ||
| Yes (1 Flap necrosis, 1 Marginal necrosis, 1 Haematoma) | 3 | 5.66% |
| No | 50 | 94.34% |
| Post-operative collections | ||
| Seroma | 1 | 1.89% |
| Hematoma | 1 | 1.89% |
| No collection | 51 | 96.22% |
| Mesh infection | ||
| Yes | 0 | 0.00% |
| No | 53 | 100.00% |
| Re-exploration of the wound | ||
| Required | 3 | 5.66% |
| Not required | 50 | 94.34% |
| Recurrence of hernia | ||
| Yes | 0 | 0.00% |
| No | 53 | 100.00% |
| Cosmetic appearance of the wound (from the patient’s perspective) | ||
| Not good | 1 | 1.89% |
| Good | 15 | 28.30% |
| Very good | 37 | 69.81% |
Table 5: General data
Discussion
Out of all primary, recurrent, and recurrent hernia, incisional and ventral hernia repair remains a challenging domain of abdominal wall surgery due to the high recurrence rates, postoperative complications, and lack of consensus on the optimal surgical approach. In our single-center series of 53 patients, most repairs 47, 88.68%) were performed via open onlay premuscular meshplasty technique, with a smaller proportion using a hybrid laparoscopic approach 6, 11.32%). The mean age of patients (48.62 ± 15.00 years) and predominance of female patients 33, 62.26%) were comparable to previous studies on incisional hernia demographics.[3,4] Our study demonstrated a mean body mass index of 32.03 ± 6.02, with 18 (33.96%) overweight and 31 (58.49%) obese. This reflects the strong association of obesity with incisional hernia occurrence and recurrence risk, as consistently highlighted in the literature.[5]
Longer hernia duration, more than 36 months in 30 (56.60%), was also notable, underlining the delay in presentation and management in our population. Operative outcomes were generally favorable. The mean hospital stay was 2.09 ± 1.12 days, with most patients discharged within 2 to 3 days. Drain duration averaged 9.56 ± 7.34 days, slightly longer than the intervals reported in some laparoscopic series, but consistent with open onlay premuscular meshplasty repairs, where subcutaneous dissection is more extensive.[5,6] Postoperative morbidity was low; wound complications were seen in 3 (5.66%), seroma in 1 (1.89%), hematoma in 1 (1.89%), and no mesh infections were reported. These results compare favourably with meta-analyses reporting wound complication rates of 10 to 20% in onlay premuscular meshplasty repairs, which is further evidenced by Clavien–Dindo classification (Table 6).[3,6]
| Complication/ Event | Number of patients (n=53) | Clavien–Dindo grade | Remarks |
| Postoperative breathlessness: Mild (conservative management) | 5 (9.43%) | Grade I | Managed without invasive intervention |
| Postoperative pain: Moderate (requiring analgesics only) | 14 (26.42%) | Grade I | No long-term sequelae, resolved with medication |
| Wound complications: Flap necrosis, marginal necrosis, hematoma (managed conservatively or minor bedside intervention) | 3 (5.66%) | Grade II | Required pharmacological/ minor wound care |
| Seroma (aspiration not required, resolved spontaneously) | 1 (1.89%) | Grade I | Conservative management |
| Hematoma (resolved without reoperation) | 1 (1.89%) | Grade I | No invasive procedure required |
| Re-exploration of the wound (surgical intervention under anesthesia) | 3 (5.66%) | Grade IIIb | Required surgical re-exploration of the wound |
| Cosmetic dissatisfaction (not good appearance, no treatment required) | 1 (1.89%) | Not applicable | Patient-reported outcome, not a complication as per Clavien–Dindo |
| Mesh infection | 0 (0.00%) | 0 | None |
| Recurrence of hernia | 0 (0.00%) | 0 | None |
Table 6: Post-operative complications according to Clavien–Dindo classification
Importantly, no hernia recurrences were observed during the follow-up period, although our relatively short to intermediate follow-up limits the ability to conclude about long-term durability. Literature suggests recurrence rates after onlay premuscular meshplasty range from 10 to 20% over 5 to 10 years.[4,7] The absence of recurrence in our series may reflect standardized technique, surgeon expertise, and careful patient selection, though extended follow-up is warranted. From a patient-centered perspective, cosmetic satisfaction was high, with 52 (98.11%) rating outcomes as good or very good. This aligns with recent reviews emphasizing the importance of cosmesis and quality of life as secondary endpoints in hernia surgery.[8] Strengths of our study include a standardized operative technique performed by a single experienced surgeon and detailed recording of both clinical and cosmetic outcomes. Limitations include the retrospective design, small sample size, lack of a direct comparison group (e.g., inlay, sublay, or laparoscopic repair), and relatively short follow-up, which precludes definitive conclusions on recurrence.
Overall, our findings suggest that open onlay premuscular meshplasty remains a safe and effective option in resource-limited settings, with low morbidity and satisfactory early outcomes; however, given the growing body of evidence favoring sublay or minimally invasive approaches for reduced wound morbidity and improved long-term durability.[3,5,6] Future prospective, randomized studies are required to clarify further the optimal strategy for primary, recurrent, and recurrent hernia repair.
Interpretation: The findings of this study suggest that open onlay premuscular meshplasty for primary, recurrent, or recurrent hernias provides favorable short-term outcomes with minimal morbidity. The absence of mesh infections and recurrences highlights the safety and effectiveness of this approach when performed with standardized technique and meticulous perioperative care. The relatively low complication rates 5 (3 (5.66%) wound complications, 1 (1.89%) seroma, and 1 (1.89%) hematoma) and high patient-reported cosmetic satisfaction in 52 (98.11%) reinforce the reliability of the procedure in all primary, recurrent, and re-recurrent hernia cases. The mean hospital stay of 2.09 ± 1.12 days and the mean drain duration of 9.56 ± 7.34 days indicate acceptable recovery time. These results align with published evidence that emphasizes the utility of onlay premuscular meshplasty in situations where inlay, sublay, or laparoscopic techniques are less feasible due to patient comorbidities, prior surgeries, or resource constraints. However, the retrospective nature and limited sample size necessitate cautious interpretation, as longer follow-up may reveal late recurrences or mesh-related complications not captured in this study.
Conclusion
Our study demonstrated that open onlay premuscular meshplasty for primary, recurrent, and recurrent hernias is a safe and effective approach, particularly in resource-limited settings. The technique was associated with low rates of wound complications in 5 (3 (5.66%) wound complications, 1 (1.89%) seroma, and 1 (1.89%) hematoma), no mesh infections, and high cosmetic satisfaction in 52 (98.11%) good to very good. Importantly, no recurrences were observed during the follow-up period. These favorable outcomes are likely attributable to standardized surgical technique and surgeon expertise. However, the retrospective design, limited sample size, and absence of a control group restrict the generalizability of findings. Long-term follow-up is essential to determine durability, especially given the known risk of recurrence in primary, recurrent, and recurrent hernia repair. Overall, our results support open onlay premuscular meshplasty as a reliable option for primary, recurrent, and recurrent hernias, while future prospective comparative studies are warranted to validate its efficacy against inlay, sublay, and minimally invasive techniques.
References
- Yewande A, Merle C, Sosin M, Mahan M, Bhanot P. Mesh and plane selection: a summary of options and outcomes. Plast Aesthet Res. 2020;7:5. doi:10.20517/2347-9264.2019.39
Crossref | Google Scholar - Karrech A, Ahmad H, Hamdorf JM. Biomechanical stability of hernia-damaged abdominal walls. Sci Rep. 2023;13(1):4936. doi:10.1038/s41598-023-31674-w
PubMed | Crossref - Pereira C, Gururaj S. Onlay Versus Sublay Mesh Repair for Incisional Hernias: A Systematic Review. Cureus. 2023;15(1):e34156. doi:10.7759/cureus.34156
PubMed | Crossref | Google Scholar - Köckerling F. Onlay Technique in Incisional Hernia Repair-A Systematic Review. Front Surg. 2018;5:71. doi:10.3389/fsurg.2018.00071
PubMed | Crossref | Google Scholar - Goodney PP, Birkmeyer CM, Birkmeyer JD. Short-term outcomes of laparoscopic and open ventral hernia repair: a meta-analysis. Arch Surg. 2002;137(10):1161-1165. doi:10.1001/archsurg.137.10.1161
PubMed | Crossref | Google Scholar - Chaouch MA, Dougaz MW, Daghmouri A, Jerraya H, Mehdi. Onlay versus sublay mesh repair of open ventral incisional hernia: a meta-analysis of randomized controlled trials. Clin Surg Res Commun. 2020;4(2):1-9. doi:10.31491/CSRC.2020.06.049
Crossref | Google Scholar - Köckerling F. Recurrent Incisional Hernia Repair-An Overview. Front Surg. 2019;6:26. doi:10.3389/fsurg.2019.00026
PubMed | Crossref | Google Scholar - Shah DK, Patel SJ, Chaudhary SR, Desai NR. Comparative study of onlay versus sublay mesh repair in the management of ventral hernias. Updates Surg. 2023;75(7):1991-1996. doi:10.1007/s13304-023-01532-5
PubMed | Crossref | Google Scholar
Acknowledgments
Not reported
Funding
None
Author Information
Corresponding Author:
Jitenkumar H Panchal
Department of General Surgery
Blue Bell Clinic, Piplod, Surat, Gujarat, India
Email: jitenkumarpanchal@gmail.com
Co-Authors:
Fasahat Hussain
Assistant Professor,
Narayan Medical College and Hospital, Jamuhar, Bihar, India
Pooja Magendra, Kanu Priya, Urwashi Rai
Post Graduate Resident
Narayan Medical College and Hospital, Jamuhar, Bihar, India
Authors Contributions
All authors contributed to the conceptualization, investigation, and data curation by acquiring and critically reviewing the selected articles. They were collectively involved in the writing – original draft preparation and writing – review & editing to refine the manuscript.
Informed Consent
Informed consent was obtained from all participating patients.
Conflict of Interest Statement
The authors declare no conflict of interest.
Guarantor
None
DOI
Cite this Article
Panchal JH, Hussain F, Magendra P, Priya K, Rai U. A Study for Clinical Outcomes of Open Hernia Repair with Onlay Premuscular Meshplasty in a Primary/ Recurrent/ Re Recurrent Hernia: A Single Centre Experience. medtigo J Med. 2025;3(4):e3062343. doi:10.63096/medtigo3062343 Crossref









