Author Affiliations
Abstract
Primary pulmonary follicular lymphoma (PPFL) is an exceptionally rare subtype of non-Hodgkin lymphoma that arises within the lung parenchyma without nodal or extrapulmonary involvement at diagnosis. Its nonspecific clinical and radiological presentation often mimics more common pulmonary diseases, leading to diagnostic delays. We report the case of a 64-year-old woman with a history of diabetes, hypertension, and cutaneous systemic lupus erythematosus (SLE) who presented with a persistent cough lasting one month. She denied constitutional symptoms, and physical examination as well as routine laboratory investigations were unremarkable. Chest X-ray and computed tomography (CT) of the thorax revealed multiple bilateral pulmonary nodules. Initial bronchoscopy and biopsy were inconclusive. Due to persistent symptoms and radiological findings, a repeat CT-guided lung biopsy was performed, which demonstrated malignant lymphoid infiltration. Immunohistochemical staining was positive for CD20, CD10, B-cell lymphoma 2 (Bcl-2), paired box protein 5 (Pax-5), and leukocyte common antigen (LCA), consistent with grade 2 follicular lymphoma. Based on these findings, a diagnosis of primary pulmonary follicular lymphoma was established. This case highlights the importance of including PPFL in the differential diagnosis of chronic pulmonary nodules, emphasizes the diagnostic value of repeat tissue sampling in inconclusive cases, and underscores the role of multidisciplinary evaluation in achieving an accurate diagnosis.
Keywords
Primary pulmonary follicular lymphoma, Infectious lung disease, Autoimmune comorbidity, Chronic pulmonary disease, Computed tomography guided biopsy.
Introduction
Primary pulmonary lymphomas (PPLs) are rare neoplasms that constitute less than 1% of all primary pulmonary malignancies and approximately 3 to 4% of extranodal lymphomas.[1,2] Among these, primary pulmonary follicular lymphoma (PPFL) is exceptionally uncommon, accounting for a small subset of PPLs and presenting diagnostic challenges due to its nonspecific clinical and radiological features.[3] Unlike the more commonly encountered nodal follicular lymphoma, PPFL often presents without extrapulmonary involvement, making it a distinct clinical entity.[4]
The pathogenesis of PPFL remains poorly understood, though it is believed to arise from ectopic lymphoid tissue within the lung, possibly secondary to chronic antigenic stimulation.[5] Patients are asymptomatic, and the disease is frequently discovered incidentally through imaging studies conducted for unrelated reasons. Radiological findings may mimic infectious, inflammatory, or other malignant conditions, often delaying diagnosis.
Case Report
A 64-year-old female with a medical history of hypertension, diabetes mellitus, and cutaneous SLE presented with a one-month chronic cough. She did not have unintentional weight loss, chills, fever, night sweats, or lymphadenopathy in the axillae, neck, or groin. She did ot smoke and had no previous lung disease and no known contact with tuberculosis (TB).
Physical examination and vital signs were unremarkable. Laboratory tests, including full blood count, liver function, and renal function, were at normal levels. Chest X-ray revealed multiple bilateral nodular opacities. (Figure 1) Sputum testing for Mycobacterium tuberculosis, including TB GeneXpert and culture, was negative. Despite completing a course of antibiotics, her symptoms and radiographic findings persisted.
Contrast-enhanced computed tomography (CECT) of the thorax demonstrated multiple bilateral pulmonary nodules of varying sizes, some with irregular and lobulated margins. (Figure 2) Bronchoscopy appeared normal, and the bronchoalveolar lavage (BAL) was negative for M. tuberculosis on culture, direct smear, and polymerase chain reaction (PCR). BAL cytology was also negative for malignancy.
There was no indication of cancer in the first CT-guided lung biopsy, which showed a heterogeneous lymphocytic infiltrate. Due to persistent symptoms and unchanged imaging, a multidisciplinary team (MDT) recommended a repeat biopsy. The second CT-guided biopsy demonstrated malignant lymphoid cells diffusely positive for leukocyte common antigen (LCA), CD20, Pax5, Bcl2, and CD10, with scattered Bcl6 positivity (Figures 3 and 4). These findings were consistent with grade 2 pulmonary follicular lymphoma. The patient was then referred to the hematological team and started chemotherapy.
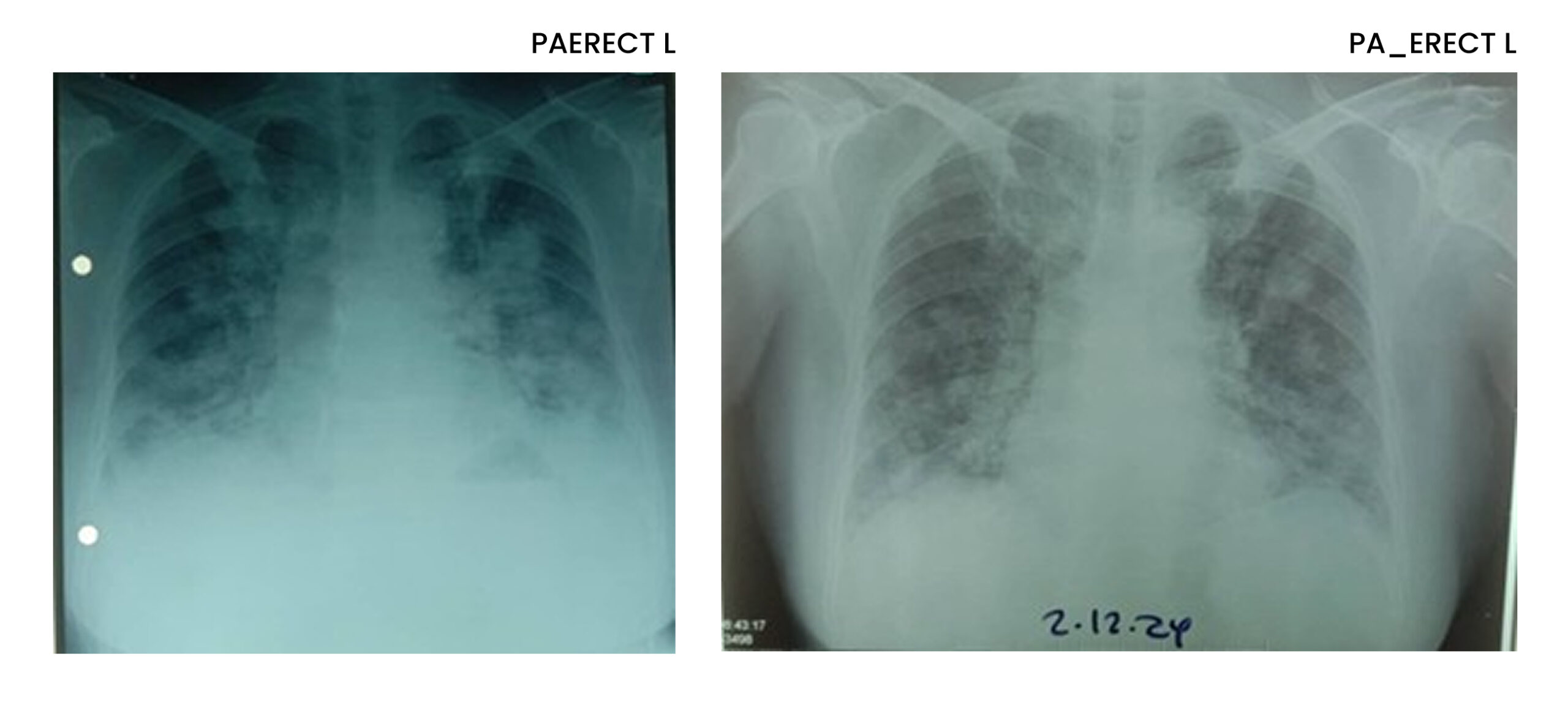
Figure 1: CXR multiple bilateral nodular opacities
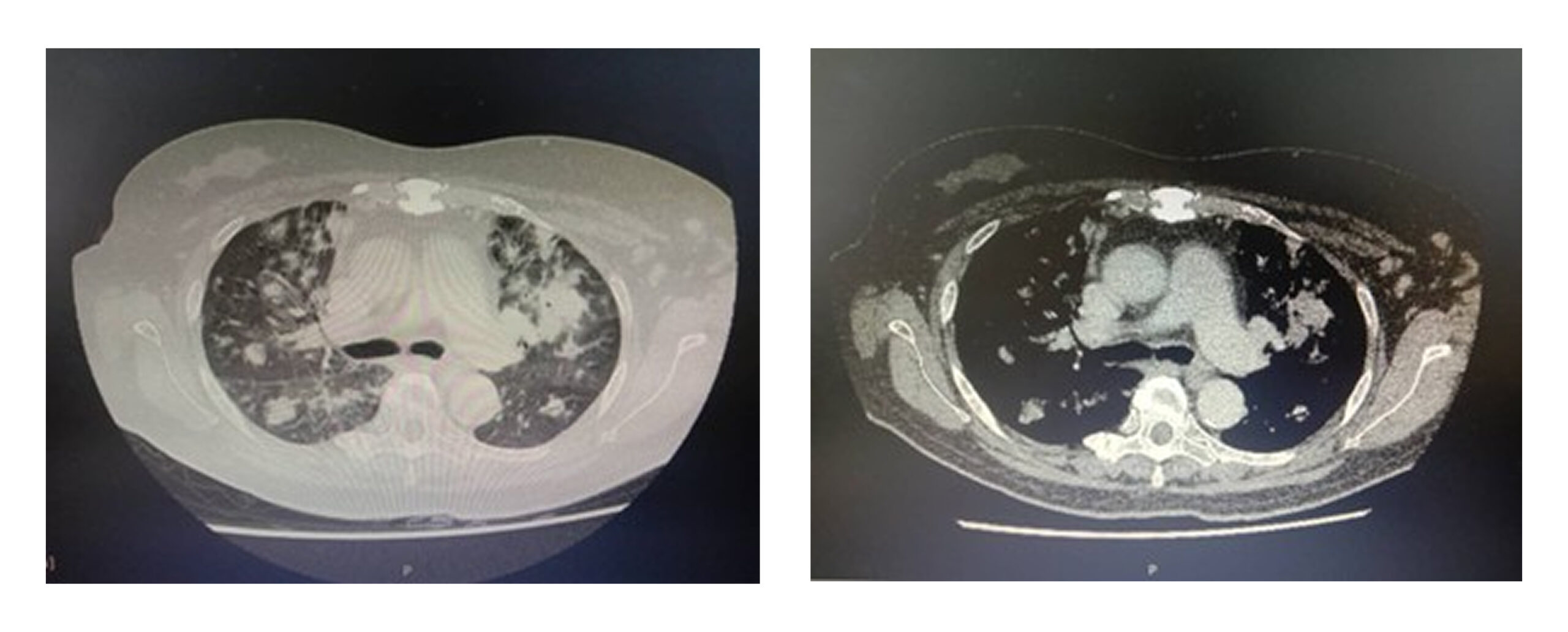
Figure 2: Multiple bilateral pulmonary nodules of varying sizes
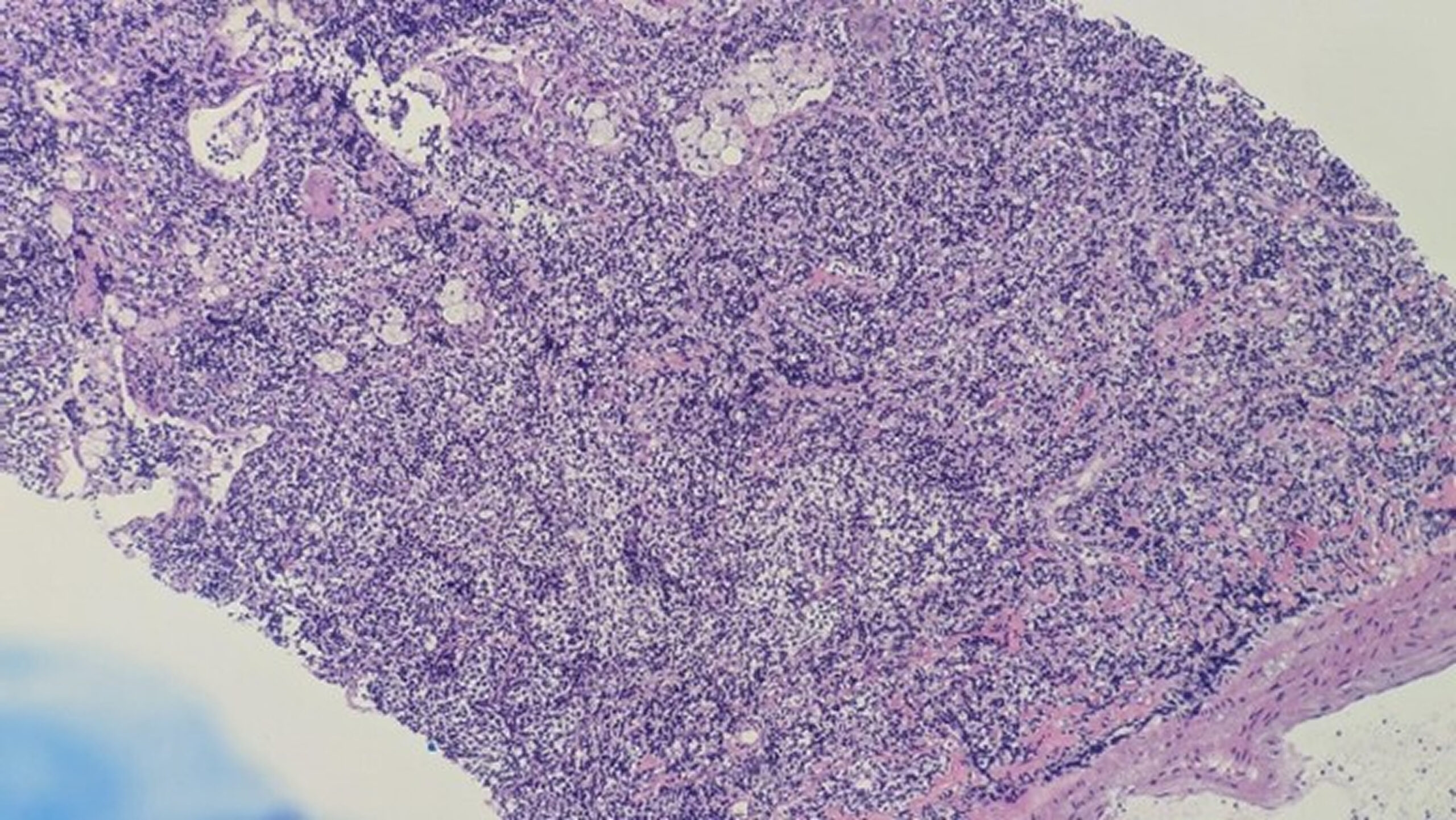
Figure 3: Vague follicular pattern (shown by arrow)
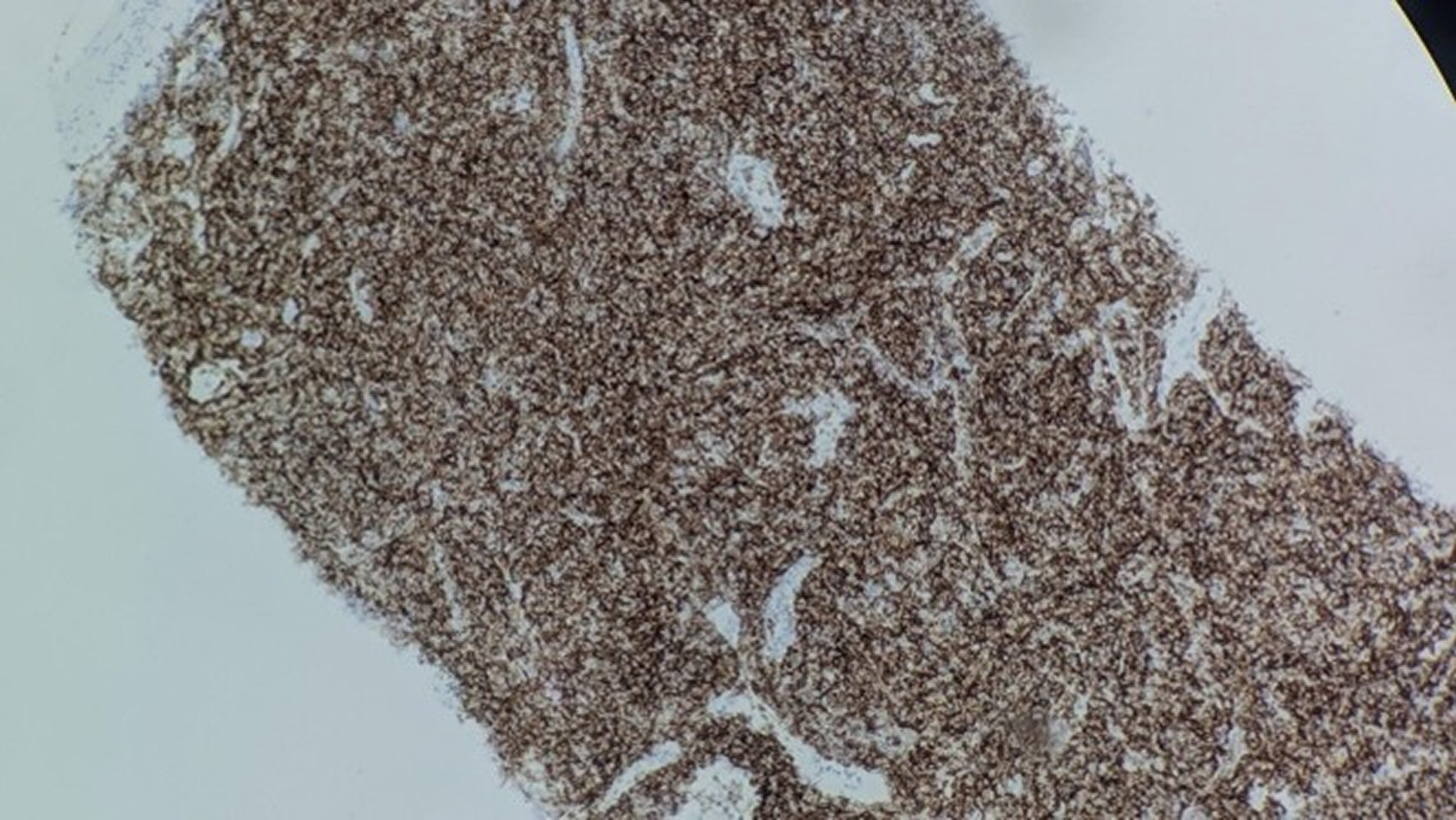
Figure 4: positive for cd20
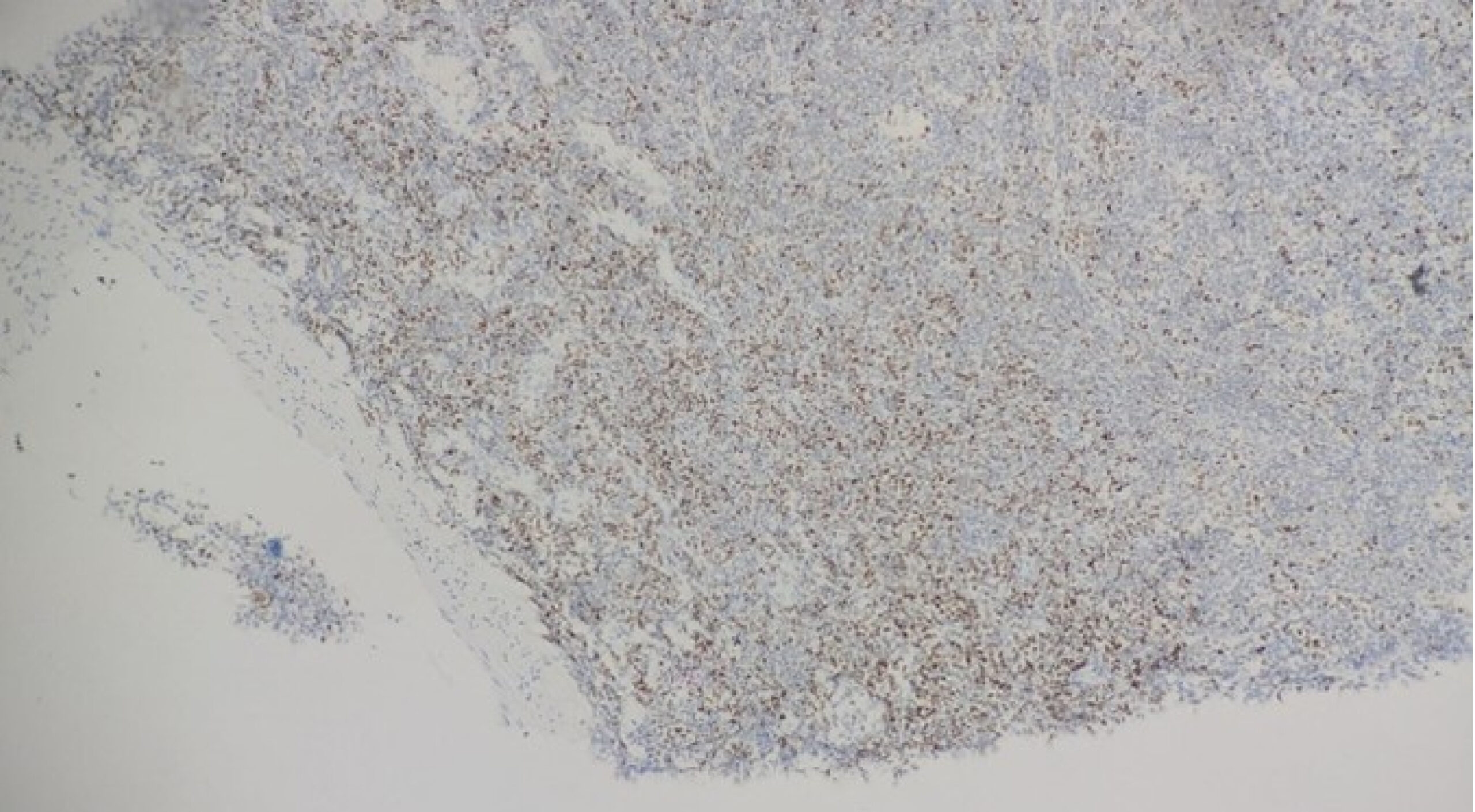
Figure 5: Bcl6 positive
Figure 3 shows the histopathological examination (HPE) revealing a vague follicular pattern (indicated by the arrow). Figure 4 shows a positive stain for CD20, and Figure 5 shows a weak positive stain for Bcl6.
Discussion
PPFL is a rare form of extra-nodal non-Hodgkin lymphoma (NHL) that originates in the lung parenchyma without initial involvement of lymph nodes or other organs. It accounts for less than 1% of all primary pulmonary lymphomas (PPLs), and the most prevalent subtype is marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue (MALT).[1] The indolent nature of PPFL, combined with nonspecific clinical and radiological features, contributes to diagnostic challenges and frequent misdiagnosis as infections, autoimmune diseases, or metastatic malignancy.
Our patient presented with a non-resolving cough and bilateral nodular lung opacities, mimicking infectious or inflammatory conditions. The absence of constitutional B symptoms and lymphadenopathy further obscured the diagnosis. Notably, the patient had a background of cutaneous SLE, an autoimmune condition known to predispose patients to lymphoproliferative disorders, including NHL.[6]
Initial diagnostic workup, including bronchoscopy and BAL, was unrevealing. Similarly, the first CT-guided biopsy revealed a benign lymphocytic infiltrate. This highlights a key pitfall in diagnosing PPFL: the potential for inadequate tissue sampling to miss diagnostic features due to the patchy nature of lymphoid infiltrates. Only after a repeat biopsy was performed did immunohistochemistry reveal a profile consistent with follicular lymphoma (CD20+, CD10+, Bcl2+, Pax5+, LCA+), confirming grade 2 PPFL.
Radiologically, PPFL may present as solitary or multiple pulmonary nodules or masses with air bronchograms, often without cavitation or lymphadenopathy.[7] PET-CT and bone marrow biopsy are recommended to exclude systemic disease, confirming the diagnosis of true PPFL.
This case underscores the importance of considering PPFL in patients with persistent pulmonary nodules unresponsive to conventional treatment, particularly when initial biopsies are non-diagnostic. Multidisciplinary discussion and repeated tissue sampling are often essential for accurate diagnosis. Early recognition is crucial, as PPFL generally has a favorable prognosis and may be managed conservatively or with immunochemotherapy depending on disease burden and symptoms.[2]
Conclusion
In summary, there are limited case reports on primary pulmonary follicular lymphoma in the literature. To the best of our knowledge, this is the first documented case of primary lung follicular lymphoma in an adult in Southern Malaysia. This underscores the importance of thorough history-taking and pursuing further investigations in patients to ensure accurate diagnosis.
References
- Cadranel J, Wislez M, Antoine M. Primary pulmonary lymphoma. Eur Respir J. 2002;20(3):750-762. doi:10.1183/09031936.02.00404102
PubMed | Crossref | Google Scholar - Cordier JF, Chailleux E, Lauque D, et al. Primary pulmonary lymphomas. A clinical study of 70 cases in nonimmunocompromised patients. Chest. 1993;103(1):201-208. doi:10.1378/chest.103.1.201
PubMed | Crossref | Google Scholar - Goodlad JR, Krajewski AS, Batstone PJ, et al. Primary cutaneous follicular lymphoma: a clinicopathologic and molecular study of 16 cases in support of a distinct entity. Am J Surg Pathol. 2002;26(6):733-741. doi:10.1097/00000478-200206000-00006
PubMed | Crossref | Google Scholar - Majid N, Kamal el B, Oncology B, Rachid A, Hassan IH. Primary pulmonary lymphoma: About five cases and literature review. Lung India. 2014;31(1):53-55. doi:10.4103/0970-2113.125909
PubMed | Crossref | Google Scholar - Isaacson PG, Du MQ. MALT lymphoma: from morphology to molecules. Nat Rev Cancer. 2004;4(8):644-653. doi:10.1038/nrc1409
PubMed | Crossref | Google Scholar - Smedby KE, Hjalgrim H, Askling J, et al. Autoimmune and chronic inflammatory disorders and risk of non-Hodgkin lymphoma by subtype. J Natl Cancer Inst. 2006;98(1):51-60. doi:10.1093/jnci/djj004
PubMed | Crossref | Google Scholar - Angirish B, Sanghavi P, Jankharia B. Pulmonary manifestations of lymphoma: A pictorial essay. Lung India. 2020;37(3):263-267. doi:10.4103/lungindia.lungindia_200_19
PubMed | Crossref | Google Scholar
Acknowledgments
The authors would like to express their sincere gratitude to Dr. Rozanah Abd Rahman, Consultant in the Department of Respiratory Medicine at Hospital Sultanah Aminah, Johor Bahru, and Dr. Lim Suet Yee, Consultant in the same department, for their invaluable guidance, support, and expertise throughout this study.
Funding
No funding
Author Information
Corresponding Author:
Hemalatha Munusamy
Department of Respiratory Medicine
Sultanah Aminah Hospital, Johor Bahru, Malaysia
Email: hemz_25@hotmail.com
Co-Author:
Rozanah Abd Rahman
Department of Respiratory Medicine
Sultanah Aminah Hospital, Johor Bahru, Malaysia
Authors Contributions
Hemalatha Munusamy served as the main author, responsible for the conception, design, data collection, analysis, and manuscript preparation. Rozanah Abd Rahman acted as the supervisor, providing guidance, oversight, and critical revisions throughout the research process and manuscript development.
Informed Consent
Informed consent was taken from the patient.
Conflict of Interest Statement
The authors declare no conflict of interest.
Guarantor
None
DOI
Cite this Article
Munusamy H, Abd Rahman R. A Silent Intruder: Case Report of Primary Pulmonary Follicular Lymphoma Mimicking Infectious Lung Disease in a Patient with Autoimmune Comorbidities. medtigo J Med. 2025;3(4):e3062346. doi:10.63096/medtigo3062346 Crossref









