Author Affiliations
Abstract
Rectal prolapse and caecal volvulus are uncommon gastrointestinal pathologies, and their simultaneous occurrence is exceedingly rare. This case highlights the importance of recognizing uncommon presentations that occur simultaneously. We describe the case of a woman in her 60s with a history of appendectomy who presented with acute abdominal pain, rectal bleeding, and rectal prolapse. Computed tomography confirmed the diagnosis of caecal volvulus, prompting prompt surgical intervention. Intraoperatively, right colectomy was performed, leading to successful recovery. This case highlights the importance of thoroughly examining all symptoms and underscores the potential underlying mechanisms or predisposing factors, such as previous abdominal surgeries, that may contribute to the coexistence of these rare conditions.
Keywords
Rectal prolapse, Caecal volvulus, Acute abdominal pain, C-reactive protein, Computed tomography.
Introduction
Rectal prolapse typically presents with rectal bleeding and protrusion of the rectal mucosa, while caecal volvulus manifests with acute abdominal pain and vomiting. The simultaneous occurrence of these two conditions is exceptionally rare, with only a few cases reported in the literature.[1,2]
Rectal prolapse is a relatively common condition, with an estimated incidence of 2.5 per 100,000 population per year. In contrast, caecal volvulus is a rare cause of intestinal obstruction, accounting for approximately 1-1.5% of all intestinal obstructions.[3,4] The coexistence of these two pathologies in a single patient is an uncommon clinical scenario that requires prompt recognition and management to prevent serious complications. Potential predisposing factors or underlying mechanisms that may contribute to the simultaneous occurrence of rectal prolapse and caecal volvulus include previous abdominal surgeries, such as appendectomy, which may alter the normal anatomical relationships and predispose the patient to these rare events.[3,5]
Case Presentation
A woman in her 60s, with a history of appendectomy in the second decade of her life, presented to the emergency department with severe right lower quadrant abdominal pain and rectal bleeding. On examination, she had diffuse abdominal tenderness and a rectal prolapse.
Blood investigations revealed a C-reactive protein (CRP) of 56 mg/L, with no leucocytosis or abnormalities in arterial blood gases. A subsequent abdominal computed tomography (CT) scan showed a loop of bowel with characteristic “coffee bean” morphology extending from the right iliac fossa towards the left upper quadrant, containing formed stool and gas, consistent with a diagnosis of caecal volvulus (Figure 1).
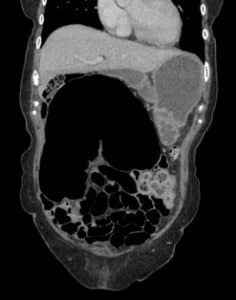

Figure 1. CT images of the abdomen showing the “coffee bean” morphology indicative of caecal volvulus
Rectal prolapse and abdominal pain occurring together may be indicative of various underlying conditions. Chronic constipation can weaken the supportive tissues of the rectum, leading to prolapse, while the straining associated with constipation can also cause abdominal discomfort. [10] Pelvic floor dysfunction, characterized by weakness or coordination issues in the pelvic muscles, can contribute to both prolapse and abdominal discomfort.[11] Complications of rectal prolapse, such as incarceration or strangulation, can lead to significant abdominal pain requiring urgent medical attention.[12] Inflammatory bowel diseases like Crohn’s disease or ulcerative colitis may cause inflammation and damage in the rectum and colon, resulting in both prolapse and abdominal pain.[13] Additionally, pelvic inflammatory conditions, neurological disorders affecting bowel function, tumours, or masses in the pelvic or abdominal region, and traumatic injuries to the pelvic area can all contribute to the simultaneous occurrence of rectal prolapse and abdominal pain.[9,15,16,17] However, the characteristic CT findings, particularly the “coffee bean” sign, led to the definitive diagnosis of caecal volvulus. While these conditions were initially considered, the CT findings ultimately ruled them out in favour of the diagnosis of caecal volvulus.[6,7]
Case Management
The patient was promptly referred to the acute surgical team, who, following review, consented the patient for surgery. Intraoperatively, the surgeons found the caecum twisted upon itself, resulting in bowel obstruction. A right hemicolectomy was performed to remove the affected portion of the colon. This surgical approach was chosen due to the presence of bowel necrosis, which precluded the option of detorsion and cecopexy.[8]
Postoperatively, the patient was hospitalized for six days. Follow-up visits typically involved physical examinations, laboratory tests, and imaging studies as needed.[19] The primary goals of the follow-up were to ensure complete recovery, monitor for any signs of recurrence or complications, and provide necessary support and guidance for the patient’s return to daily activities and work.[20] The patient’s health continued to improve progressively during follow-up. She gradually resumed daily activities and work, transitioning from light tasks to full duties. The follow-up period typically lasts several weeks to months, depending on the patient’s individual circumstances and the surgeon’s recommendations.[21] During this time, the patient may be advised to follow specific dietary guidelines, engage in light physical activity, and attend physical therapy sessions if necessary.[22]
Surveillance and monitoring guidelines for patients who have undergone a right hemicolectomy for caecal volvulus typically involve regular follow-up appointments, imaging studies (such as CT scans or colonoscopies), and laboratory tests to detect any potential complications or recurrence [18]. The frequency and duration of these follow-up visits may vary based on the patient’s age, overall health, and risk factors.[19]
It is essential to adhere to the recommended follow-up schedule and guidelines to ensure optimal recovery and early detection of any potential issues.[18] Prompt intervention and appropriate management can help prevent further complications and improve the patient’s overall outcome.
Discussion
The simultaneous presentation of rectal prolapse and caecal volvulus is extremely rare, with only a handful of documented cases in the medical literature.[1] This case presents a unique clinical scenario of these two rare conditions coexisting in a patient with a history of appendectomy, which may suggest potential predisposing factors or underlying pathophysiological mechanisms.
A review of the literature reveals that there are only a few documented cases of concurrent rectal prolapse and caecal volvulus, underscoring the rarity of this clinical presentation. The challenges in establishing clear criteria or guidelines for managing such rare, simultaneous presentations are evident, as the available literature is limited to case reports. Previous case reports by Barussaud et al. (2005) emphasized the necessity of prompt surgical intervention, while Steinberg et al. (2014) emphasized the importance of considering rare pathologies in management.[1,2]
Prompt diagnosis and intervention are paramount in managing such cases to prevent complications like bowel ischemia and necrosis. In this instance, timely surgical consultation and imaging studies, particularly a CT scan, facilitated accurate diagnosis and appropriate management. The CT findings, including the characteristic “coffee bean” sign indicative of caecal volvulus, effectively guided the surgical team in planning the intervention. While the CT scan is a valuable diagnostic tool, it is essential to acknowledge that there may be limitations or potential pitfalls in its interpretation, particularly in rare presentations such as this one.[6,7]
| LEARNING POINTS/TAKE HOME MESSAGES |
|
Surgical management of caecal volvulus typically involves detorsion of the bowel and measures to prevent recurrence, such as enteropexy or right hemicolectomy, depending on the intraoperative findings. In this case, the surgeons encountered a twisted caecum resulting in bowel obstruction, leading to the decision to perform right colectomy to remove the affected segment of the colon and prevent future recurrences.
Conclusion
In conclusion, the presented case underscores the significance of recognizing the rare coexistence of rectal prolapse and caecal volvulus, highlighting the importance of thorough evaluation in patients presenting with acute abdominal pain and rectal bleeding. Timely diagnosis, aided by imaging studies and prompt surgical intervention, is crucial in managing simultaneous rectal prolapse and caecal volvulus to prevent serious complications. While the patient in this case responded well to surgical treatment, further research is needed to better understand the potential underlying mechanisms and predisposing factors that may contribute to the coexistence of rectal prolapse and caecal volvulus, which could inform the development of more comprehensive management strategies for this uncommon clinical scenario.
References
- Barussaud ML, Mantoo S, Wyart V, Meurette G, Lehur PA. The magnetic anal sphincter in faeca l incontinence: is initial success sustained over time? Colorectal Dis. 2013;15(12):1499-1503. doi:10.1111/codi.12423 PubMed | Crossref |
Google Scholar - Cavazzoni E, Rosati E, Zavagno V, Graziosi L, Donini A. Simultaneous Delorme’s procedure and inter-sphincteric prosthetic implant for the treatment of rectal prolapse and faecal incontinence: preliminary experience and literature review. Int J Surg. 2015;14:45-48. doi:10.1016/j.ijsu.2014.12.031 PubMed | Crossref | Google Scholar
- Madiba TE, Baig MK, Wexner SD. Surgical management of rectal prolapse. Arch Surg. 2005;140(1):63-73. doi:10.1001/archsurg.140.1.63 PubMed | Crossref | Google Scholar
- Rabinovici R, Simansky DA, Kaplan O, Mavor E, Manny J. Cecal volvulus. Dis Colon Rectum. 1990;33(9):765-769. doi:10.1007/BF02052323 PubMed | Crossref | Google Scholar
- Raveenthiran V, Madiba TE, Atamanalp SS, De U. Volvulus of the sigmoid colon. Colorectal Dis. 2010;12(7 Online):e1-e17. doi:10.1111/j.1463-1318.2010.02262.x PubMed | Crossref | Google Scholar
- Delabrousse E, Sarliève P, Sailley N, Aubry S, Kastler BA. Cecal volvulus: CT findings and correlation with pathophysiology. Emerg Radiol. 2007;14(6):411-415. doi:10.1007/s10140-007-0647-4 PubMed | Crossref | Google Scholar
- Rosenblat JM, Rozenblit AM, Wolf EL, DuBrow RA, Den EI, Levsky JM. Findings of cecal volvulus at CT. Radiology. 2010;256(1):169-175. doi:10.1148/radiol.10092112 PubMed | Crossref | Google Scholar
- Consorti E, Liu T. Diagnosis and treatment of caecal volvulus. Postgrad Med J. 2005;81(962):772-776. doi:10.1136/pgmj.2005.035311 PubMed | Crossref | Google Scholar
- Yang MS, Lee SH, Kim TW, et al. Epidemiologic and clinical features of anaphylaxis in Korea. Ann Allergy Asthma Immunol. 2008;100(1):31-36. doi:10.1016/S1081-1206(10)60401-2 PubMed | Crossref | Google Scholar
- Wald A, Bharucha AE, Cosman BC, Whitehead WE. ACG clinical guideline: management of benign anorectal disorders. Am J Gastroenterol. 2014;109(8):1141-1157. doi:10.1038/ajg.2014.190 PubMed | Crossref | Google Scholar
- Norton C, Cody JD. Biofeedback and/or sphincter exercises for the treatment of faecal incontinence in adults. Cochrane Database Syst Rev. 2012;2012(7):CD002111. doi:10.1002/14651858.CD002111.pub3 PubMed | Crossref |
Google Scholar - Bordeianou L, Hicks CW, Kaiser AM, Alavi K, Sudan R, Wise PE. Rectal prolapse: an overview of clinical features, diagnosis, and patient-specific management strategies. J Gastrointest Surg. 2014;18(5):1059-1069. doi:10.1007/s11605-013-2427-7 PubMed | Crossref | Google Scholar
- Adams DH. Sleisenger and Fordtran’s Gastrointestinal and Liver Disease. Gut. 2007;56(8):1175. doi:10.1136/gut.2007.121533 Sleisenger and Fordtran’s Gastrointestinal and Liver Disease
- Nelson RL, Abcarian H, Davis FG, Persky V. Prevalence of benign anorectal disease in a randomly selected population. Dis Colon Rectum. 1995;38(4):341-344. doi:10.1007/BF02054218 Prevalence of benign anorectal disease in a randomly selected population
- Rao SS. Constipation: evaluation and treatment. Gastroenterol Clin North Am. 2003;32(2):659-683. doi:10.1016/s0889-8553(03)00026-8 Constipation: evaluation and treatment
- Tsunoda A. Surgical treatment of rectal prolapse in the laparoscopic era: a review of the literature. J Anus Rectum Colon. 2020;4(3):89-99. doi:10.23922/jarc.2019-035 PubMed | Crossref
- Kehlet H, Wilmore DW. Multimodal strategies to improve surgical outcome. Am J Surg. 2002;183(6):630-641. doi:10.1016/s0002-9610(02)00866-8 PubMed | Crossref | Google Scholar
- David et al. National Comprehensive Cancer Network. Colorectal cancer screening. J Natl Compr Canc Netw. 2013;11(12):1538-1575. doi:10.6004/jnccn.2013.0180 PubMed | Crossref | Google Scholar
Acknowledgments
Not reported
Funding
Not reported
Author Information
Sumaiya Amin Adrita
Department of Emergency Medicine
Maidstone & Tunbridge Wells NHS Trust
Email: sumaiya.adrita@nhs.net
Author Contribution
The author contributed to the conceptualization, investigation, and data curation by acquiring and critically reviewing the selected articles and was involved in the writing – original draft preparation and writing – review & editing to refine the manuscript.
Informed Consent
The patient provided written informed consent for the publication of this case report, including the use of anonymized clinical data and images. All patient information has been de-identified to protect privacy.
Conflict of Interest Statement
Not reported
Guarantor
None
DOI
Cite this Article
Sumaiya AA. A Case of Simultaneous Rectal Prolapse and Caecal Volvulus. medtigo J Emerg Med. 2024;1(1):e3092111. doi:10.63096/medtigo3092111 Crossref









