Author Affiliations
Abstract
Background: Scimitar syndrome, also known as Veno-lobar syndrome, is a rare congenital malformation described by partial anomalous pulmonary venous return (PAPVR) from the right lung to the inferior vena cava (IVC). This condition is often associated with right lung hypoplasia or agenesis, presenting significant diagnostic challenges due to its similarity to other pulmonary conditions.
Case presentation & management: We report the case of a 20-year-old asymptomatic female who was initially misdiagnosed with pulmonary tuberculosis (TB) based on incidental findings of right lung volume loss during a pre-travel medical evaluation. Following a month of anti-TB treatment without symptom resolution, advanced imaging studies revealed scimitar syndrome, highlighting the importance of differential diagnosis in similar cases.
Conclusion: This case underscores the necessity of considering congenital anomalies like scimitar syndrome in the differential diagnosis of unilateral lung abnormalities, particularly in endemic regions for TB. Accurate diagnosis is critical for effective management and optimal long-term outcomes.
Keywords
Scimitar syndrome, Partial anomalous pulmonary venous return, Congenital anomalies, Pulmonary tuberculosis, Differential diagnosis.
Introduction
Scimitar syndrome is a rare congenital heart defect characterized by an aberrant venous return from the right lung, typically draining into the IVC, often accompanied by structural abnormalities such as hypoplasia or agenesis of the right lung. First described in 1836 by the French physician Henri de Lannelongue, the name “scimitar” derives from the curved shape of the anomalous vein resembling a scimitar sword.[1,2] While the condition is often diagnosed in infancy, many patients remain asymptomatic until adulthood, complicating clinical presentations and diagnostic pathways.[3,4]
Misdiagnosis of scimitar syndrome as pulmonary TB is common in areas where TB prevalence is high, as both conditions can manifest with similar radiographic findings, such as volume loss in the affected lung.[5] This report highlights the critical need for heightened awareness of congenital anomalies in patients presenting with unexplained lung abnormalities, particularly in endemic regions for TB.[6]
Case Presentation
A 20-year-old female presented to the institution seeking a second opinion after being diagnosed with pulmonary TB at an external facility. This diagnosis was made following an incidental finding of right lung volume loss during a routine medical evaluation required for international travel. The external facility initiated anti-TB therapy based solely on radiological findings, prescribing a standard regimen including isoniazid, rifampicin, ethambutol, and pyrazinamide. However, after one month of treatment, the patient reported no resolution of her symptoms, which included persistent fatigue and a mild, dry cough.
On further inquiry, the patient reported no history of fever, night sweats, or significant weight loss, and her body mass index was within normal limits of 21.32. There was no notable past medical history, including previous respiratory infections, and her family history was unremarkable concerning pulmonary diseases.
Physical examination: Upon examination, the patient appeared well-nourished, in no acute distress, and demonstrated stable vital signs. The respiratory examination revealed decreased breath sounds on the right side and normal chest wall excursion without any signs of wheezing or crackling. Cardiac examination was unremarkable, showing a regular rate and rhythm without murmurs.
Investigations: Initial chest radiography revealed right lung volume loss and ipsilateral mediastinal displacement, raising suspicion for venous anomalies (Figure 1). A contrast-enhanced chest computed tomography (CT) scan was then performed, confirming the diagnosis of scimitar syndrome. The imaging demonstrated an anomalous right pulmonary vein draining into the IVC, associated with hypoplasia of the right lung (Figure 2, Figure 3, Figure 4). Additionally, two-dimensional transthoracic echocardiography was conducted to evaluate for any associated cardiac anomalies, which were not detected. An abdominal ultrasound was performed to assess liver size and anatomical relationships, yielding unremarkable results.

Figure 1: Chest X-ray
Hypoplastic right lung with ipsilateral mediastinal shift and shadow of the anomalous pulmonary vein seen as a tubular structure paralleling the right heart border (blue arrow pointing to the tubular structure).

Figure 2: Chest CT
A linear scimitar shape opacity running from the midline of the lung toward the diaphragm (shown as arrow).
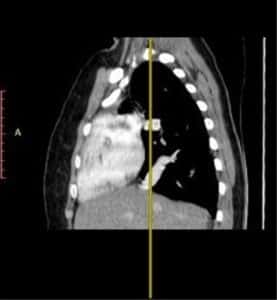
Figure 3: Chest CT
Sagittal view of the thorax showing a linear scimitar-shaped opacity.
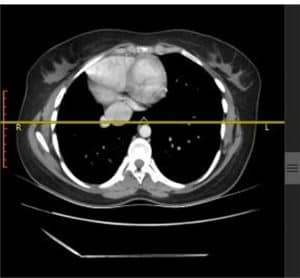
Figure 4: Chest CT
Showing the lower part of the aberrant venous drainage into IVC (arrowhead PV, arrow IVC).
Discussion
Scimitar syndrome presents unique diagnostic challenges, particularly in adult patients, where its manifestations can be subtle and easily confused with more prevalent conditions like pulmonary TB. The characteristic imaging findings: an anomalous right pulmonary vein and right lung hypoplasia are essential for diagnosis, but can be obscured by concurrent respiratory conditions.[7] The initial misdiagnosis in our patient emphasizes the necessity for clinicians to maintain a broad differential diagnosis when evaluating patients with unilateral lung abnormalities. This case exemplifies the importance of a thorough history, physical examination, and judicious use of imaging studies to differentiate congenital anomalies from infectious diseases.[8,9] In areas with high TB prevalence, awareness of scimitar syndrome is particularly important, as misdiagnosis can lead to unnecessary treatment, increased healthcare costs, and patient distress.
Management strategies for scimitar syndrome depend on the severity of the clinical presentation and associated anomalies. While asymptomatic patients may require only monitoring, symptomatic individuals often necessitate surgical intervention to correct the anomalous drainage and alleviate respiratory symptoms. Surgical options may include re-implantation of the pulmonary vein into the left atrium or, in some cases, a lobectomy if hypoplasia is significant.[10,11] Long-term follow-up is crucial to monitor for potential complications such as pulmonary hypertension (HTN), respiratory infections, and exercise intolerance, which can significantly impact quality of life.[12]
Conclusion
This case underscores the critical importance of accurate diagnosis in the management of congenital anomalies such as scimitar syndrome, particularly in regions where pulmonary TB is a common diagnosis. The findings advocate increased education and awareness among healthcare professionals to improve diagnostic accuracy and patient outcomes, thereby facilitating timely and appropriate interventions.
References
- Gupta ML, Bagarhatta R, Sinha J. Scimitar syndrome: A rare disease with unusual presentation. Lung India. 2009;26(1):26-29. doi:10.4103/0970-2113.45202 PubMed | Crossref | Google Scholar
- Benjouad I, Taam I, El Ataouna K, et al. Scimitar syndrome: about a case and review of the literature. Pan Afr Med J. 2016;25:37. doi:10.11604/pamj.2016.25.37.10545 PubMed | Google Scholar
- Chowdhury UK, Anderson RH, Sankhyan LK, et al. Surgical management of the scimitar syndrome. J Card Surg. 2021;36(10):3770-3795. doi:10.1111/jocs.15857 PubMed | Crossref | Google Scholar
- Gunasekera KS, Vonasek B, Oliwa J, et al. Diagnostic challenges in childhood pulmonary tuberculosis—Optimizing the clinical approach. Pathogens. 2022;11(4):382. doi:10.3390/pathogens11040382 PubMed | Crossref | Google Scholar
- Baxter R, McFadden PM, Gradman M, Wright A. Scimitar syndrome: cine magnetic resonance imaging demonstration of anomalous pulmonary venous drainage. Ann Thorac Surg. 1990;50(1):121-123. doi:10.1016/0003-4975(90)90101-b PubMed | Crossref | Google Scholar
- Kahrom M, Kahrom H. Scimitar syndrome and evolution of managements. Pan Afr Med J. 2009;3:20. Scimitar syndrome and evolution of managements
- Luknár M, Hlivák P, Lesný P, Goncalvesová E. Scimitar syndrome in adulthood: challenges in management and individualized approaches. Cureus. 2024;16(6):e61857. doi:10.7759/cureus.61857 Crossref | Google Scholar
- Dyer KT, Hlavacek AM, Meinel FG, et al. Imaging in congenital pulmonary vein anomalies: the role of computed tomography. Pediatr Radiol. 2014;44(9):1158-1157. doi:10.1007/s00247-014-3044-7 PubMed | Crossref | Google Scholar
- Cheng W, Li Z, Zhu Y, et al. Surgical correction for scimitar syndrome by right thoracotomy and direct anastomosis in children. Pediatr Investig. 2021;5(1):46-51. doi:10.1002/ped4.12255 PubMed | Crossref | Google Scholar
- Matsuyama Y, Saigusa N, Hioki M, et al. A case of partial anomalous pulmonary venous return to inferior vena cava and left atrium (Scimitar syndrome). Nihon Kyobu Geka Gakkai Zasshi. 1994;42(1):144-9. A case of partial anomalous pulmonary venous return to inferior vena cava and left atrium (Scimitar syndrome)
- Geggel RL, Gauvreau K, Callahan R, Feins EN, Baird CW. Scimitar syndrome: A new multipatch technique and incidence of postoperative pulmonary vein obstruction. JTCVS Tech. 2020;4:208-216. doi:10.1016/j.xjtc.2020.07.027 PubMed | Crossref | Google Scholar
- Dusenbery SM, Geva T, Seale A, Valente AM, Zhou J, Sena L, Geggel RL. Outcome predictors and implications for management of scimitar syndrome. Am Heart J. 2013;165(5):770-777. doi:10.1016/j.ahj.2013.01.016 PubMed | Crossref | Google Scholar
Acknowledgments
We extend our gratitude to Dr. Yeraeifire Sileshi, CEO of Saglan Wajee General Hospital, for his unwavering support in this case.
Funding
Not reported
Author Information
Corresponding Author:
Henok Baharu Wodajeneh
Department of Internal Medicine
Saglan Wajee General Hospital, Ethiopia
Email: h0913129050@gmail.com
Co-Authors:
Tigist Desta Beyera
Department of Internal Medicine
Armauer Hansen Research Institute, Ethiopia
Ashenafi Tesfaye Bedada
Department of General Surgery
Menelik II Specialized Hospital, Ethiopia
Ashenafi Negash Tekle
Department of Orthopedics and Traumatology
St. Paul’s Hospital Millennium Medical College, Ethiopia
Kebron Yihenew Getnet
Department of Medicine
Jigjiga Karamara General Hospital, Ethiopia
Eyosias Lemma Teshome
Department of Internal Medicine
Assistant Professor of Internal Medicine, Hemato-oncology Fellow
St. Paul’s Hospital Millennium Medical College, Ethiopia
Fikadu Tolesa Kabeta and Tamiru Alemu Degaga
Department of Internal Medicine
Saglan Wajee General Hospital, Ethiopia
Eyerusalem Yalew Talemma
Department of Internal Medicine
Zewditu Memorial Hospital, Ethiopia
Authors contributions
All authors contributed to the conceptualization, investigation, and data curation by acquiring and critically reviewing the selected articles. They were collectively involved in the writing – original draft preparation, and writing – review & editing to refine the manuscript. Additionally, all authors participated in the supervision of the work, ensuring accuracy and completeness. The final manuscript was approved by all named authors for submission to the journal.
Informed Consent
The patient provided informed consent.
Conflict of Interest Statement
Not reported
Guarantor
None
DOI
Cite this Article
Henok BW, Tigist DB, Ashenafi TB, et al. A Case of Scimitar Syndrome Misdiagnosed as Pulmonary Tuberculosis: A Rare Congenital Anomaly with Implications for Clinical Practice. medtigo J Med. 2024;2(4):e30622455. doi:10.63096/medtigo30622455 Crossref









